Should you or a loved one have a spinal cord injury, you may observe swelling in the legs or difficulty moving—common signs of edema, where fluid accumulates due to disrupted circulation. This can occur after trauma, surgery, or prolonged immobility, leaving you feeling stiff and uncomfortable. But comprehending the causes, from pressure on spinal nerves to infections, helps you spot warnings sooner. Simple steps like elevating your legs or wearing compression socks can alleviate symptoms while improving daily comfort—there’s more to investigate on managing this condition effectively.
Common Causes of Spinal Cord Edema
Even whenever you’re managing a spinal cord injury well, swelling in your legs—spinal cord edema—can sneak up on you.
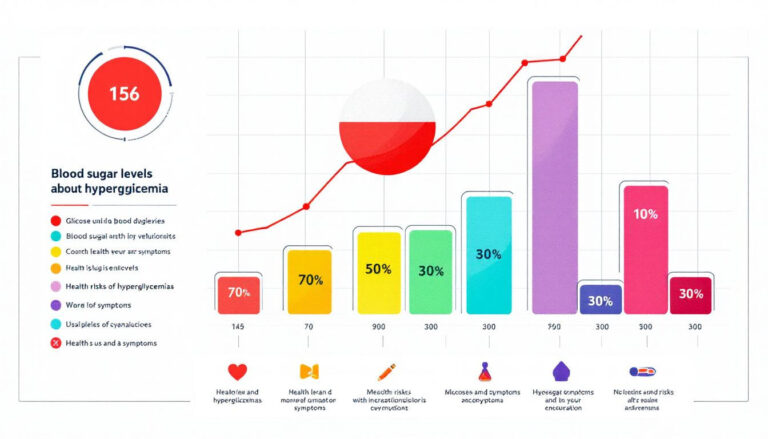
After spinal cord injuries, paralysis often leads to physical inactivity, causing fluid pooling in your lower limbs. Gravity pulls fluids down, and without movement, they don’t circulate properly. Dehydration or sudden sodium changes can make things worse, throwing off your body’s balance.
Whenever left unchecked, this swelling raises risks like skin breakdown from constant pressure or deep vein thrombosis from poor blood flow.
Watching your diet—especially cutting back on salty foods—helps keep fluid levels steady. Simple shifts, like elevating your legs or using compression gear, can ease the strain.
Staying proactive with small changes makes a big difference in keeping edema under control.
Recognizing Symptoms of Spinal Cord Edema
Spotting the signs of spinal cord edema promptly can help take action before complications set in. You may notice swelling, especially in your legs, as fluid pools due to decreased nerve function.
Pay attention to decreased sensation—like numbness or tingling—in your arms or legs, which can signal pressure on the spinal cord.
Should you be struggling with bowel or bladder control, it could mean edema is affecting nerve signals.
Watch for burning pain or weakness in your limbs, as these are red flags.
Don’t ignore skin changes; poor sensation increases your risk of unnoticed injury.
Prompt recognition means better results, so listen to your body.
In the event that these symptoms appear after a spinal cord injury, seek help fast. Quick action protects your mobility and comfort.
Diagnostic Approaches for Spinal Cord Edema
To diagnose spinal cord edema, you’ll likely start with an MRI, which shows swelling and rules out other issues.
Your doctor will also check your symptoms, like weakness or numbness, to understand how the edema affects you.
A thorough neurological exam helps pinpoint the exact impact on your movement and sensation, guiding the next steps in your care.
MRI Imaging Techniques
Several MRI imaging techniques can help pinpoint spinal cord edema, giving doctors a clear view of what’s happening inside your body. These scans identify abnormalities like fluid buildup or tissue swelling, guiding treatment strategies.
Here’s how MRI works for spinal cord edema:
- T2-weighted imaging: Highlights hyperintense (bright) areas, showing where fluid has accumulated in the spinal cord.
- Diffusion-weighted imaging: Measures water movement, revealing subtle damage or inflammation.
- Contrast-enhanced MRI: Uses a dye to spot leaks or blood vessel issues causing edema.
- Sagittal and axial views: Provides cross-sections of your spine, helping doctors see compression or misalignment.
MRI’s detailed imaging guarantees prompt identification, so you get the right care faster. It’s painless and non-invasive, making it a safe choice for diagnosing spinal cord edema.
Clinical Symptom Assessment
| Red Flags | What to Check | Why It Matters |
|---|---|---|
| Sudden leg weakness | Muscle strength tests | Signals nerve compression |
| Numbness/tingling | Sensory exam | Indicates spinal cord pressure |
| Swelling below injury | Visual/physical check | Points to fluid buildup |
| Mobility issues | Range-of-motion tests | Reveals motor function loss |
Regular monitoring is key—early action improves results. Trust your instincts and consult a specialist if these signs match.
Neurological Examination Methods
- ASIA classification: Tests muscle strength and sensation to map nerve damage on a standardized scale.
- Vital signs check: Blood pressure and heart rate are monitored—especially for autonomic issues like sudden drops (dysreflexia).
- Imaging (MRI/CT): Scans reveal swelling severity and pinpoint compressed areas in the spinal cord.
- Continuous monitoring: Detects changes in movement, sensation, or reflexes, catching complications promptly.
This structured approach helps tailor care to your needs, whether it’s rehab or emergency intervention.
You’re not alone—these steps guide your recovery.
Immediate and Long-Term Care Strategies
Even though swelling in your legs feels overwhelming after a spinal cord injury, small daily steps can make a big difference.
Start by elevating your legs for 15 minutes a few times daily—this helps reduce fluid retention. Wear compression stockings to support circulation and keep swelling down.
Stay hydrated by drinking at least 8 cups of water daily; it helps your body manage fluids better. Cut back on salty foods since too much sodium worsens swelling.
Should moving be hard, ask a caregiver or therapist to help with passive range of motion exercises—gentle movements keep blood flowing.
These habits, done consistently, ease discomfort and prevent long-term issues. You’ve got this—every small effort adds up to real relief.
Rehabilitation and Physical Therapy Options
You can improve circulation and reduce swelling with range of motion exercises, where a therapist or caregiver helps move your legs should you be unable to do it yourself.
Functional electrical stimulation (FES) bikes also activate your leg muscles, boosting blood flow and keeping edema under control.
These therapies work best whenever you stick with them regularly, so they become part of your routine.
Range of Motion Exercises
Keeping joints moving is key during managing edema after a spinal cord injury—gentle range of motion exercises help your body stay flexible while easing swelling.
These exercises combat limited mobility by improving blood flow and reducing fluid pooling in your limbs. Here’s how they work:
- Passive Movements: A caregiver or therapist gently moves your joints for you, keeping them loose and encouraging circulation.
- Active-Assistive Exercises: You use your stronger muscles to help move weaker limbs, boosting fluid movement.
- Consistency Matters: Doing these exercises multiple times a day prevents stiffness and supports edema management.
- Full Motion: Moving joints through their natural range maintains muscle tone and prevents long-term stiffness.
Functional Electrical Stimulation
Because managing edema after a spinal cord injury can feel overwhelming, Functional Electrical Stimulation (FES) offers a promising way to regain movement and reduce swelling.
FES uses gentle electrical pulses to activate muscles, which helps improve blood circulation and prevent fluid buildup in your limbs. This not only eases edema but also strengthens muscle tone, making daily activities easier.
For those with spinal cord injuries, regular FES sessions can boost mobility and lower risks like blood clots. It’s often paired with other therapies for a well-rounded approach.
You’ll work with a therapist to tailor the intensity, ensuring it’s safe and effective. Over time, FES could help you feel more in control of your body, easing discomfort and improving your quality of life.
Preventive Measures to Minimize Edema Risk
While handling spinal cord injuries can make managing fluid retention tricky, there are simple steps you can take to lower the risk of edema.
By staying proactive, you can keep swelling under control and avoid complications. Here’s how:
- Elevate your legs above heart level for 15 minutes a few times daily—this helps fluid move back to your heart.
- Stay hydrated with at least 8 cups of water a day to balance fluid levels and reduce retention.
- Try cardiovascular exercise like arm cycling or seated workouts 3-4 times weekly to boost circulation.
- Wear compression stockings to gently squeeze veins, preventing fluid buildup in your legs.
Don’t forget daily body inspections to spot initial signs of swelling or skin issues, especially when sensation is limited.
These small habits make a big difference.