You may not expect groin pain after back surgery, but it’s more common than you realize—and the reasons behind it are surprisingly interconnected. Should you be feeling discomfort in your groin post-surgery, it could stem from nerve irritation, inflammation from healing tissues, or even how your body compensates for changes in movement. Comprehending these causes can help you take the right steps toward relief, so let’s analyze what could be going on.
Nerve Compression and Radicular Pain Pathways
Should you have undergone back surgery and now experience groin pain, nerve compression could be the culprit.
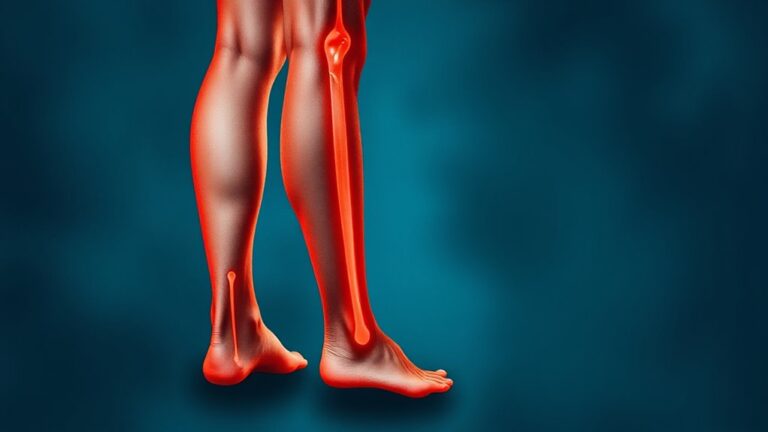
During spinal surgery, nearby nerves might get squeezed, leading to radicular pain—sharp, shooting discomfort that travels down your groin or leg.
In case you’ve had spinal fusion, scar tissue (adhesions) can form, irritating nerve roots and causing lingering pain.
Studies show 10-40% of patients deal with new or worse symptoms post-surgery, often due to unresolved nerve issues.
To pinpoint the problem, doctors use imaging studies like MRIs to spot compression or adhesions. Effective diagnosis helps guide targeted interventions, such as nerve blocks or physical therapy, to ease irritation.
Don’t ignore persistent groin pain—it’s a sign your nerves need attention. Prompt action improves recovery, so talk to your doctor about next steps.
Inflammation and Scar Tissue Formation Impact
After back surgery, inflammation and scar tissue can sneak in and stir up trouble, particularly should you be feeling groin pain. Inflammation is your body’s natural response to surgery, but at the time it lingers, it can cause swelling and irritation in nearby tissues, including your groin.
Scar tissue, or adhesions, can form around the surgical site, sticking to nerves or muscles and creating discomfort. This can lead to compensatory movements—like favoring one side—that strain your groin and worsen pain.
Scar tissue can bind to nerves or muscles, causing discomfort and altered movement that strains the groin.
Physical therapy helps by breaking down scar tissue and easing inflammation, speeding up recovery. Gentle stretches, anti-inflammatory meds, and targeted exercises can reduce tissue stiffness and improve mobility.
Don’t ignore persistent pain—early intervention makes a big difference in your comfort and healing.
Altered Biomechanics and Muscle Imbalances
Because your body naturally adapts after back surgery, altered movement patterns can throw off your balance—literally.
Limited spinal function forces you to move differently, shifting stress to areas like your hip flexors and groin. These compensatory movements create muscle imbalances, where some muscles work too hard while others weaken.
Over time, this strain on the groin leads to pain, especially in the event that your spinal mobility isn’t fully restored. Changes in movement patterns also tighten certain muscles, pulling unevenly on your pelvis.
Targeted rehabilitation approaches can help by rebalancing strength and flexibility. Pain management strategies, like gentle stretches and core exercises, ease discomfort by correcting these imbalances.
The key is recognizing how altered biomechanics affect your body and addressing them promptly.
Aggravation of Pre-Existing Conditions
Back surgery doesn’t just change your spine—it can stir up trouble in areas you didn’t expect, especially in case you already had fundamental pelvic or hip issues.
Should you have had sacroiliac joint problems or other pelvic conditions before spinal fusion, the surgery could worsen them. The biomechanical load shifts after fusion, forcing your hips and pelvis to bear more stress.
This can trigger compensatory movement patterns, like favoring one side, which strains your groin or hips even more. Posture alteration from surgery also redistributes pressure, aggravating pre-existing imbalances and leading to persistent pain.
In case your hip pain was misdiagnosed as back pain before surgery, it could flare up afterward. Recognizing these connections helps you address the root cause instead of just masking symptoms.
Post-Surgical Rehabilitation Challenges
Rehabilitation after back surgery can take longer than one anticipates, especially in the event that you’re managing groin pain that slows your progress.
Managing pain effectively is key, but finding the right balance between rest and movement can be tricky at the time discomfort flares up.
Your recovery timeline depends on factors like your body’s healing response and how well you adhere to your rehab plan.
Rehabilitation Duration Factors
While you could expect your recovery after back surgery to follow a straightforward timeline, several factors can actually stretch it out longer than anticipated.
Your rehabilitation duration depends on your age, overall health, and whether you’d pelvic pain or other issues before surgery. Complications like mobility limitations or adjacent segment disease can slow progress, and persistent groin or pelvic pain could mean a longer recovery.
A thorough pre-op assessment helps tailor your rehab plan, but unexpected setbacks still happen.
- Pain levels: High post-op pain can delay mobility exercises.
- Pre-existing conditions: Pelvic pain or weak muscles might need extra attention.
- Complications: Infections or nerve issues add time to recovery.
- Comprehensive approach: A personalized rehab plan speeds up healing.
Stay patient—your body heals at its own pace.
Pain Management Strategies
Managing pain after back surgery doesn’t have to feel like an uphill battle—there are proven ways to ease discomfort and get you moving again.
Should you have had spinal fusion surgery and struggle with hip pain, start with physical therapy to strengthen muscles and correct movement patterns.
Non-steroidal anti-inflammatory drugs (NSAIDs) can help reduce inflammation, but always follow your doctor’s advice.
Don’t overlook psychological support; stress and frustration can make pain feel worse, so mindfulness or support groups may assist.
Thorough evaluations pinpoint the root of your pain, so you get targeted rehabilitation strategies.
Small steps, like gentle stretches or walking, improve mobility and quality of life.
Stay patient—your body’s healing, and these pain management strategies will guide you toward recovery.
Diagnostic and Treatment Strategies for Relief
For treatment strategies, conservative approaches often come initially:
- Physical therapy to strengthen muscles and improve flexibility.
- Pain relief methods like anti-inflammatory meds to reduce inflammation.
- Steroid injections should the pain persists.
- As a last resort, surgical interventions to fix foundational problems.
Staying patient and following your care plan can help you recover faster.
Consistency with your treatment plan and patience will speed up your recovery process.
Always communicate openly with your doctor to adjust treatments as needed.
Conclusion
Visualize your nerves after surgery like a garden hose squeezed underfoot—pressure in one spot can make water sputter far away. That’s how nerve compression in your back can fire pain signals to your groin. But just like untangling the hose, targeted rehab and patience ease the kinks. One patient described it as “learning to walk without tripping over concealed roots.” Relief isn’t instant, but with the right steps, the path gets smoother.