Modic changes are seen on MRI scans as specific alterations in the vertebral endplates and are often associated with chronic low back pain. If you’re suffering from persistent back pain, understanding Modic changes might help you pinpoint the cause. This article breaks down what Modic changes are, their causes, types, and their impact on your spinal health.
Key Takeaways
- Modic changes are significant alterations in vertebral endplates linked to chronic low back pain, varying in prevalence based on factors such as age, sex, and genetics.
- The pathophysiology of Modic changes involves inflammation and degeneration processes, with Type 1 changes characterized by inflammation and edema, while Types 2 and 3 reflect chronic degeneration and structural alterations.
- Targeted treatments, including non-surgical options, surgical interventions, and antibiotic therapy, are essential for managing Modic changes and improving quality of life, especially given the chronic nature of these conditions.
Modic Changes
Modic changes are alterations in the vertebral body endplate on MRI scans, typically linked to degenerative disc disease. These changes are significant as they are often associated with chronic low back pain, a condition that affects a vast number of people worldwide. Dr. Michael Modic first described and classified these changes, emphasizing their importance in understanding spinal degeneration and associated pain.
The signal intensity alterations in vertebral bone marrow signal intensity seen on MRI, known as Modic changes, are classified into three types based on their distinct characteristics. These bone marrow changes can lead to increased pain and disability, highlighting their relevance in the overall understanding of spinal health, including marrow signal intensity changes and vertebral marrow edema.
Prevalence and Risk Factors
The prevalence of Modic changes among individuals with degenerative disc disease can vary widely, ranging from 19% to 59%. This variation underscores the need for awareness and understanding of these changes in the context of spinal health.
Several common risk factors have been identified:
- Male sex
- Older age
- Diabetes
- Genetic factors
- Smoking
- Obesity
- Spinal deformities
- Higher occupational loads
Among these, age stands out as a significant risk factor, with the prevalence of Modic changes increasing notably in individuals over 50 years old.
Maintaining a healthy weight is crucial in preventing Modic changes, as excess body weight increases the spinal load, contributing to potential Modic changes. Practicing good posture during daily activities can also alleviate undue stress on the spine, helping to prevent these changes.
Addressing these risk factors early can mitigate the impact of Modic changes on spinal health.
Pathophysiology of Modic Changes
The pathophysiology of Modic changes involves several key processes, primarily centered around vertebral endplate damage.
When the integrity of the vertebral endplate is compromised, it triggers a cascade of degenerative events that can lead to vertebral endplate changes, modic vertebral endplate changes, modic vertebral endplate changes, vertebral endplate signal, and vertebral endplate change.
Factors contributing to the development of these changes include:
- Endplate damage
- Disc degeneration
- Endplate and disc degeneration
- Intra-osseous pressure
- Inflammation
Increased mechanical loads on existing endplate defects can further propagate Modic changes, particularly type 2. Understanding these underlying mechanisms helps in developing strategies to prevent and treat Modic changes, which play a significant role in spinal degeneration and endplate degeneration associated pain.
Inflammatory Processes
Inflammatory processes are at the heart of Modic changes, particularly type 1, which represents bone marrow edema and inflammation, a sign of active degeneration.
In Modic type 1 changes, signs of inflammation such as granulation tissue, fibrosis, and histologic findings of bone marrow edema are evident. These inflammatory changes are often adjacent to degenerated vertebral endplates, indicating the close relationship between disc degeneration and reactive endplate marrow changes.
Proinflammatory cytokines such as TNF, IL-1, and IL-6 are activated following tissue damage in Modic changes.
Macrophages also play a significant role in these inflammatory processes by contributing to chronic inflammation and tumor necrosis factor immunoreactive responses, including necrosis factor immunoreactive cells. Persistent inflammatory stimuli are key contributors to the development and chronicity of Modic changes, exacerbating chronic low back pain and tumor necrosis factor.
The inflammation in Modic type 2 changes entails processes like fibrosis, angiogenesis, and neurogenesis, which contribute to chronic low back pain.
These fibroinflammatory changes showcase the complex interaction between inflammation and spinal degeneration, highlighting the need for targeted treatments to address these underlying inflammatory processes.
Role of Bacteria
The role of bacteria in Modic changes has garnered significant attention, particularly with the identification of Propionibacterium acnes as a potential contributor.
Disc herniation can initiate an infection that leads to Modic changes, with approximately 30-34% of patients with a disc herniation having bacteria present in the extruded disc material. These infections release metabolites that trigger inflammation, further contributing to the development of Modic changes.
Understanding the role of bacterial infections in Modic changes opens new avenues for treatment, including antibiotic therapy. This approach can be particularly beneficial for cases where bacterial infection is a contributing factor to the degenerative process.
Causes of Modic Changes
Several factors contribute to the development of Modic changes, including:
- degenerative disc disease
- spine injury or trauma
- inflammation and infection
- genetic factors
- lifestyle choices
Each of these causes plays a unique role in the progression of Modic changes, influencing the overall health and function of the human spine.
1. Degenerative Disc Disease
Degenerative disc disease is a major contributor to Modic changes, particularly due to the effects of intervertebral disc degeneration on adjacent vertebral endplates.
As discs degenerate, they can lead to increased intra-osseous pressure and metabolic changes in the vertebrae, which may trigger Modic changes. The degeneration of lumbar spinal discs, which support weight-bearing and mobility, is a significant factor in developing degenerative lumbar disk disease.
The association between disc degeneration and Modic Type 1 changes is well-documented, highlighting the role of aging in spinal health. Understanding this relationship aids in developing targeted interventions to prevent and manage Modic changes and their associated pain related to severe disc degeneration and degenerative disk disease assessment.
2. Spine Injury or Trauma
Spine injuries or trauma, such as fractures or accidents, can also trigger Modic changes. These injuries cause disruptions to the vertebral body and surrounding tissues, leading to degenerative changes. Acute injuries are often linked with immediate Modic changes, while chronic injuries may result in progressive changes over time.
The impact of trauma on spinal health underscores the need for prompt and effective treatment to prevent long-term degeneration and the development of Modic changes. Addressing these injuries early can mitigate their impact on the spine and overall health.
3. Inflammation and Infection
Inflammation plays a significant role in the development of Modic Type 1 changes, often resulting from adjacent disc degeneration. Chronic inflammatory conditions can exacerbate these changes, emphasizing the role of inflammatory processes in spinal health. Certain infections, particularly those caused by low-virulence bacteria, can lead to Modic changes by promoting inflammation in the affected areas.
Understanding the interplay between inflammation and infection is crucial for developing effective treatments for Modic changes. Targeting these underlying processes can alleviate pain and slow the progression of spinal degeneration.
4. Genetic Factors and Family History
Genetic predisposition may increase the likelihood of developing Modic changes, indicating a hereditary aspect to these conditions. Family history of spinal disorders can further elevate the risk, suggesting that inherited traits play a role in spinal health. Research on inherited spinal conditions supports the idea that genetics contribute to the susceptibility of developing Modic changes.
Recognizing the genetic factors involved in Modic changes helps identify individuals at higher risk and enables early intervention strategies.
5. Lifestyle Factors and Posture
Lifestyle factors, such as poor posture and physical activity, significantly impact spinal health and the risk of developing Modic changes. Poor posture during daily activities can place undue stress on the spine, leading to degenerative changes over time. Prolonged periods of sitting without movement can also accelerate spinal degeneration, increasing the risk of Modic changes.
Regular physical activity is crucial for maintaining spinal health and preventing Modic changes. Healthy habits and good posture can significantly reduce the risk of degenerative changes, helping to maintain overall spinal well-being.
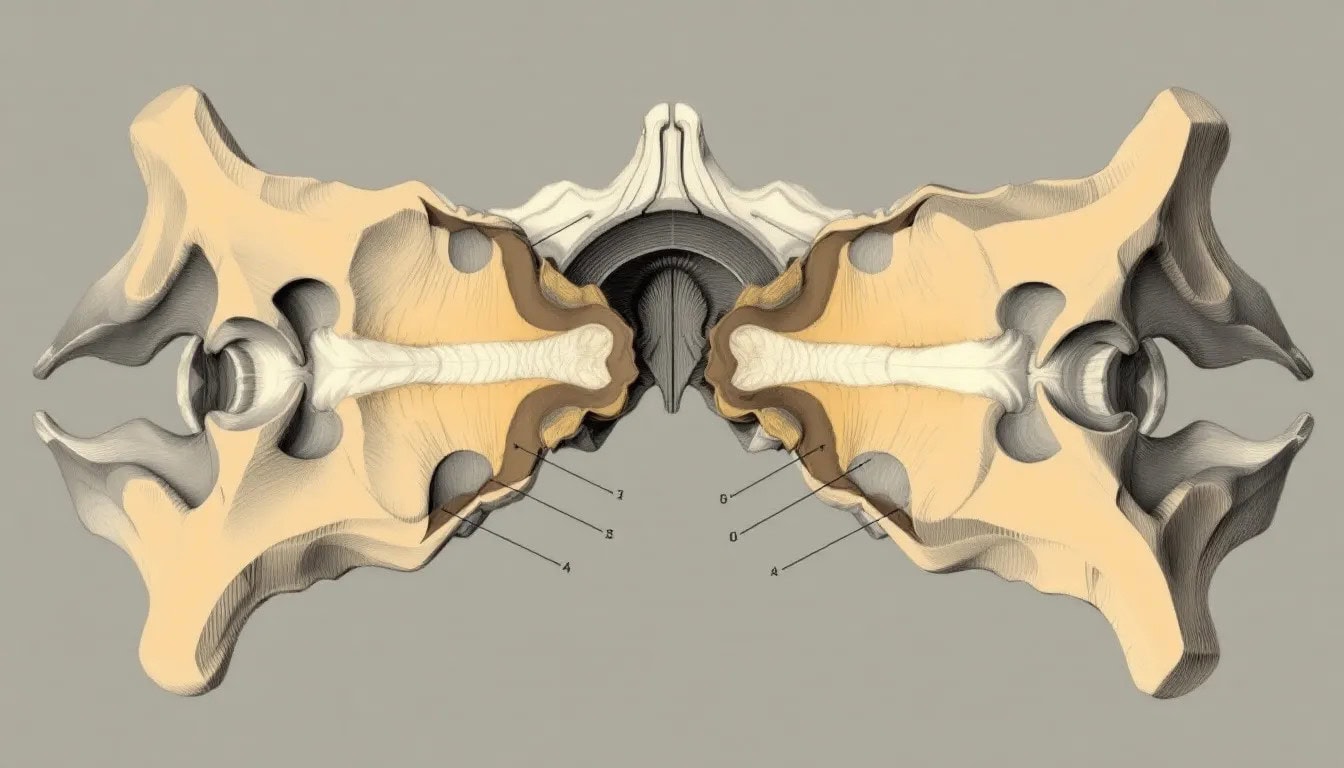
Types of Modic Changes
Modic changes are classified into three distinct types based on MRI signal characteristics observed in the vertebral body. Each type has unique features and implications for spinal health, influencing the treatment and management strategies.
1. Type 1 Modic Changes
Type 1 Modic changes are characterized by inflammation and edema in the bone marrow with mr imaging, often visible as high signal intensity on T2-weighted MRI images. Patients with Type 1 Modic changes commonly experience significant pain due to the inflammatory processes affecting the spinal structure. On MRI, these changes typically show low signal intensity on T1-weighted images and high signal intensity on T2-weighted images.
The presence of Type 1 Modic changes can be indicative of potential low-grade infection in the vertebral area. These changes are often associated with significant pain and discomfort, highlighting the need for targeted treatments to address the underlying inflammation.
2. Type 2 Modic Changes
Type 2 Modic changes signify the transformation of normal red bone marrow to yellow fatty marrow due to ischemia and fatty degeneration. These marrow changes are often associated with chronic disc degeneration, indicating long-standing issues in spinal health. Clinically, Type 2 Modic changes may present symptoms such as chronic pain and functional impairment.
On MRI, Type 2 changes appear as high signal intensity on T1-weighted images and iso to high signal on T2-weighted images. Understanding the characteristics of Type 2 Modic changes aids in developing effective treatment strategies to manage chronic pain and improve spinal health.
3. Type 3 Modic Changes
Type 3 Modic changes are indicative of sclerotic alterations in the bone, representing a more advanced stage of degeneration. These changes can lead to structural modifications in the vertebral bone, diminishing its mechanical strength and potentially leading to further complications. On MRI, Type 3 changes typically show low signal intensity on both T1 and T2-weighted images.
Unlike Types 1 and 2, Type 3 Modic changes are distinct due to their radiographic appearance and underlying pathophysiology. These sclerotic changes highlight the progression of spinal degeneration and the need for comprehensive management strategies to address the associated pain and disability.
Symptoms of Modic Changes
Modic changes are often linked to persistent discomfort in the neck and back due to spinal degeneration. These changes are frequently associated with chronic low back pain and modic conditions and can exacerbate symptom severity.
Recognizing the symptoms of Modic changes is key for timely diagnosis and effective treatment.
1. Chronic Back Pain
Modic changes contribute significantly to chronic back pain, impacting daily activities and overall quality of life. Type 1 Modic changes, in particular, can result in constant pain, especially at night, and can significantly limit daily activities. Research indicates that Type 1 Modic changes are present in approximately 4% of individuals with lower back pain.
Patients with Modic changes often report a gradual increase in the intensity and persistence of their back pain. The clinical presentation of back pain in these patients can vary significantly, affecting individual pain management strategies, underscoring the need for personalized treatment approaches.
2. Radiating Pain or Nerve Compression
Modic changes can lead to symptoms associated with nerve compression, such as radiating pain in the legs (sciatica). These changes can irritate nearby nerve roots, leading to sensations of pain radiating down the limbs. Symptoms of numbness and tingling can accompany radiating pain due to Modic changes affecting nerve pathways.
The presence of Modic type I changes has been linked with an increased risk of 9.5 immunoreactive nerve fibers compression syndromes, highlighting the need for comprehensive diagnostic and treatment strategies to address these symptoms effectively.
3. Stiffness and Limited Range of Motion
Individuals with Modic changes may experience significant stiffness that restricts their range of motion, particularly in the morning or after prolonged periods of inactivity. This stiffness can impact flexibility and movement, further complicating daily activities.
Pain associated with Modic changes can lead to compensatory movement patterns, which may exacerbate spinal instability and further limit mobility. Targeted therapies and exercises are essential for improving overall spinal health and functionality.
4. Decreased Quality of Life
Chronic pain resulting from Modic changes can lead to psychological challenges, including increased anxiety and depression. The ongoing discomfort often leads to reduced participation in social and recreational activities, impacting overall well-being and contributing to sciatic pain.
Sleep disturbances are common among individuals with Modic changes, further affecting mental and emotional health. Addressing the psychological and emotional aspects is vital for a holistic approach to managing Modic changes and improving quality of life.
Clinical Presentation and Diagnosis
Modic changes often manifest as changes in vertebral body marrow, which may correlate with chronic low back pain symptoms. However, the clinical importance of Modic changes in determining treatment options is still largely unclear, particularly in relation to lumbar vertebral bodies.
A comprehensive clinical presentation and diagnosis are crucial for effective management.
Symptoms and Physical Examination
Patients with Modic changes often experience intense and disabling low back pain episodes, with peaks of pain typically occurring late at night and in the morning. Morning stiffness is a common symptom, indicating the need for a thorough physical examination to assess spinal health.
Type 1 Modic changes suggest a possibility of lumbar instability requiring surgical intervention, particularly at the l5 s1 level. Before planning surgical treatment, the possibility of infection should be investigated to ensure appropriate management.
Imaging Techniques
MRI is essential for identifying Modic changes and distinguishing them from other spinal disorders. The specific characteristics of the endplate contour in MR imaging can help differentiate Modic changes from spondylodiscitis.
In cases of suspected infection, additional imaging such as CT and gadolinium-enhanced magnetic resonance imaging may be necessary.
Treatment Options for Modic Changes
The treatment options for Modic changes include non-surgical treatments, surgical interventions, and antibiotic therapy. While evidence on the efficacy of these treatments remains ambiguous, exploring different approaches is essential for managing chronic pain and improving patients’ quality of life.
Non-Surgical Treatments
Conventional non-surgical treatments have limited effectiveness in reducing pain for individuals with Modic changes. Certain alternative therapies, including bisphosphonates and hyperbaric oxygen, have been assessed for their effectiveness in treating Modic changes. Potential therapeutic options for Modic type 2 changes include blocking or accelerating conversions between Modic change subtypes.
Exploring these non-surgical treatments can provide valuable insights into managing Modic changes without the need for invasive procedures. Tailored approaches based on individual patient needs are crucial for optimizing treatment outcomes.
Surgical Interventions
Surgical options, including lumbar fusion, are considered for patients with Modic changes when conservative treatments fail. However, surgical outcomes for patients with type II Modic changes may also be limited, necessitating careful evaluation before intervention. Lumbar fusion typically predicts excellent outcomes following surgery, but this may vary based on the presence of Modic changes.
A thorough assessment of each case is essential to determine if surgical intervention is appropriate for patients with Modic changes, ensuring that the benefits outweigh the risks.
Antibiotic Therapy
Antibiotic therapy is being explored as a treatment option for Modic changes, particularly those linked to infections. Recent research indicates that antibiotic therapy might be beneficial in some instances of Modic changes caused by infections. This approach could open new avenues for managing Modic changes and reducing chronic pain.
Impact on Quality of Life
Modic et al changes can serve as an independent predictor of significant and debilitating low back pain episodes in patients. These changes often lead to persistent and nocturnal pain, resulting in higher levels of functional impairment compared to those without Modic changes.
Addressing these impacts is crucial for improving patients’ quality of life.
Pain Management Challenges
Patients with Modic changes often experience pain flare-ups that contribute to difficulties in achieving restful sleep. Managing pain linked to Modic changes often presents difficulties that can adversely affect patients’ sleep patterns. Effective pain management for these patients is complicated by the need for tailored treatment approaches due to individual variability in pain response.
Type 1 Modic changes are associated with a higher likelihood of lumbar instability, complicating pain management strategies and requiring comprehensive treatment plans.
Long-Term
Only a small percentage of patients with initial Modic changes show resolution after ten years, indicating the chronic nature of the condition, often linked to bacterial presence. Less chronic disability associated with Modic changes was observed in a 13-year follow-up study, suggesting that long-term outcomes can vary widely.
Individuals with Modic changes experience a longer average duration of chronic pain compared to those without these changes. Understanding the long-term outlook is crucial for developing effective management strategies and improving patient outcomes.
Preventive Measures
Addressing lumbar disc degeneration early can prevent excessive stress on the vertebral endplates, which is crucial for preventing Modic changes. Engaging in healthy habits and exercises is vital to maintain spinal health and reduce the risk of developing Modic changes related to lumbar disc herniation and lumbar spine issues.
Early Intervention Strategies
Early intervention is crucial for managing symptoms and improving long-term outcomes for patients with Modic changes. Long-term prognosis for individuals with Modic changes can vary widely, making early assessment and intervention crucial for improving outcomes.
Implementing early intervention strategies can help mitigate the impact of Modic changes on spinal health and overall well-being, emphasizing the importance of timely and proactive management.
Lifestyle Tips for Spinal Health
Prioritizing restorative sleep is crucial for overall spinal health and may help prevent Modic changes. Healthy lifestyle habits, including proper sleep, can significantly reduce the risk of developing Modic changes in the spine. Maintaining spinal health is crucial for overall well-being and helps mitigate the risks associated with chronic low back pain.
Adopting and maintaining these healthy habits can lead to long-term improvements in spinal health and quality of life, highlighting the importance of lifestyle choices in preventing Modic changes.




