The carotid body, found at the bifurcation of the common carotid artery, is essential for monitoring blood oxygen levels. It helps the body adjust breathing and cardiovascular functions in response to changes in oxygen availability. Dive into this article to learn about its anatomy, function, and significance in health and disease.
Key Takeaways
- The carotid body, located at the bifurcation of the common carotid artery, functions as a peripheral chemoreceptor, monitoring blood oxygen levels to maintain homeostasis.
- Glomus type I cells within the carotid body are essential for detecting hypoxia, initiating reflexes that adjust respiratory and cardiovascular activity to enhance oxygen delivery.
- Clinical significance includes the potential for carotid body tumors to impact surrounding structures and the association of carotid body overactivity with hypertension and metabolic disorders.
Anatomy of the Carotid Body
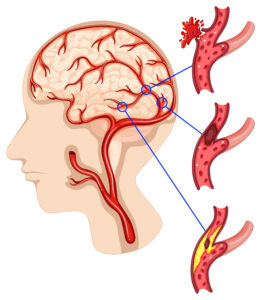
The carotid body is a small, oval-shaped organ located at the bifurcation of the common carotid artery, where it splits into the internal and external carotid arteries. This strategic position at the junction of these major arteries allows the human carotid body to effectively monitor the blood flow and the content of oxygen in the blood.
Nestled posteriorly to the bifurcation, it is ideally situated to serve its role as carotid body chemoreceptors, continuously surveying the blood for changes in oxygen levels. Comprising various cell types, the carotid body includes a rich network of blood vessels and nerves, critical for its function.
The intricate anatomy of the carotid body functions is crucial for its role in maintaining homeostasis, which we will explore further in the subsequent sections.
Glomus Cells
At the heart of the carotid body’s function are the glomus cell, which can be broadly categorized into two types: glomus type I (glomus) cells and type II (sustentacular) cells. The type I glomus cells are the primary sensory receptors, adept at detecting oxygen levels in the blood. These cells are equipped with specialized oxygen-sensitive potassium channels that play a pivotal role in the oxygen-sensing mechanism.
Surrounding these are the type II sustentacular cells, which provide structural support and maintain the microenvironment necessary for the type I cells to function optimally. Together, these supporting cells and cell types form a complex network that is integral to the carotid body’s role in monitoring and responding to changes in blood chemistry.
Blood Supply and Nerve Innervation
The carotid body receives a robust blood supply primarily from branches of the external carotid artery, with contributions from the internal carotid artery as well. This extensive vascular network ensures that the carotid body is well-perfused, allowing it to rapidly detect changes in blood gases.
Additionally, the carotid body is innervated by the carotid sinus nerve, a branch of the glossopharyngeal nerve (cranial nerve IX), and the vagus nerve (cranial nerve X). These nerves carry sensory fibers information from the carotid body to the central nervous system, where it can trigger appropriate physiological responses.
This intricate innervation and blood supply underline the carotid body’s critical role in maintaining homeostasis.
Function of the Carotid Body
The carotid body is a crucial player in regulating respiratory and cardiovascular functions by detecting changes in blood gases. As a peripheral chemoreceptor, it monitors arterial blood oxygen levels and initiates reflexes to adjust breathing and cardiovascular activity accordingly. This function is vital for maintaining the body’s homeostasis, particularly in response to hypoxia (low oxygen levels) or hypercapnia (high carbon dioxide levels), involving the cardiorespiratory centers.
When oxygen levels drop, the carotid body triggers a reflex that increases respiratory rate, cardiac output, and blood pressure to enhance oxygen delivery to tissues. Understanding this function is essential for appreciating the carotid body’s role in health and disease.
Oxygen Sensing Mechanism
The oxygen-sensing mechanism of the carotid body is primarily mediated by type I glomus cells, which are highly sensitive to changes in the partial pressure of oxygen. These cells utilize oxygen-sensitive potassium channels to detect low oxygen levels (hypoxia).
When oxygen levels drop, these channels alter the membrane potential of the glomus cells, leading to the release of neurotransmitters. This process initiates a cascade of events that ultimately signals the central nervous system to increase respiratory rate and depth, thereby improving oxygen uptake and delivery.
This sophisticated mechanism highlights the carotid body’s vital role in responding to hypoxic conditions.
Chemoreceptor Reflex Response
Beyond oxygen sensing, the carotid body also responds to changes in carbon dioxide levels and blood acidity, which are natural stimuli that influence breathing and blood pressure. When the carotid body detects hypoxia, it increases blood pressure, heart rate, and respiratory rate, thereby enhancing oxygen delivery throughout the body.
Chronic intermittent hypoxia, a condition often associated with sleep apnea, can lead to overactivity of the carotid body, resulting in elevated sympathetic nervous system activity and increased blood pressure. This heightened activity can contribute to metabolic dysfunctions such as insulin resistance and altered glucose metabolism.
Understanding these reflex responses is crucial for comprehending the carotid body’s role in health and disease.
Clinical Significance of the Carotid Body
The carotid body’s role extends beyond physiological regulation to significant clinical implications. Carotid body tumors, though generally noncancerous, can impact surrounding nerves and blood vessels if they grow larger. These tumors can alter the function of the carotid sinus and affect cardiovascular and respiratory function.
Understanding the clinical significance of the carotid body is essential for diagnosing and managing conditions that may arise from its dysfunction or pathology. The following subsections will delve into carotid body tumors and their impact on cardiovascular health.
Carotid Body Tumors
Carotid body tumors can be either benign or malignant, with the majority of most carotid body tumors being noncancerous. However, as these tumors grow, they can cause symptoms such as hoarseness, tongue numbness, and difficulty swallowing, including cases involving a carotid body tumor.
Diagnosis of these tumors often involves imaging tests like CT scans or MRIs to determine the tumor’s size and location. Surgical removal is the primary treatment approach, especially for symptomatic tumors, requiring careful dissection techniques to minimize complications such as nerve damage and significant blood loss.
Preoperative embolization can help reduce the risk of bleeding during surgery, and postoperative monitoring is crucial for assessing cranial nerve function. Understanding these aspects is vital for managing carotid body tumors effectively.
Impact on Cardiovascular Health
Overactivity of the carotid body has been linked to increased blood pressure and is a contributing factor in hypertension. During episodes of hypoxia, the carotid body enhances sympathetic nerve activity, increasing blood pressure and heart rate to ensure adequate oxygen delivery to vital organs. Chronic intermittent hypoxia can exacerbate this overactivity, leading to further cardiovascular complications.
Additionally, the carotid body’s response to hypoxia includes stimulating pathways that negatively affect glucose metabolism, potentially leading to insulin resistance and metabolic dysfunctions. Targeting carotid body activity may offer new therapeutic strategies to mitigate these conditions. Understanding this impact is crucial for developing effective treatments for cardiovascular and metabolic disorders.
Carotid Sinus and Its Role
The carotid sinus, a dilation located at the junction of the common carotid artery and the internal carotid artery, houses baroreceptors that detect blood pressure variations. These baroreceptors are critical for maintaining hemodynamic stability by sending sensory discharges to the central nervous system to regulate blood pressure.
The carotid sinus plays a pivotal role in detecting changes in blood pressure and triggering appropriate reflexes to ensure cardiovascular homeostasis. Understanding the function of the carotid sinus is essential for appreciating its role in health and disease.
Baroreceptor Function
Baroreceptors within the carotid sinus detect changes in blood pressure and send sensory signals to the central nervous system to regulate breathing and blood pressure. This baroreceptor function is crucial for maintaining cardiovascular and respiratory function, ensuring that blood flow is adequate to meet the body’s needs.
The carotid sinus’s ability to detect high arterial pressure and modulate sympathetic tone is essential for hemodynamic stability. Proper function of these baroreceptors is critical for autonomic nervous system regulation and blood pressure homeostasis.
Understanding these functions helps in diagnosing and managing conditions related to blood pressure regulation.
Carotid Sinus Syndrome
Carotid sinus syndrome is characterized by exaggerated baroreceptor responses, leading to symptoms such as fainting, dizziness, and falls. This syndrome is often triggered by pressure on the carotid sinus, which can lead to syncope due to abrupt changes in blood pressure.
Diagnosis may involve performing a carotid sinus massage to assess the heart rate and blood pressure response. Treatment options vary based on severity, ranging from lifestyle changes and medications to surgical interventions, including permanent cardiac pacing for severe cases.
Understanding these aspects is crucial for managing carotid sinus syndrome effectively.
Embryology and Development
The development of the carotid body involves contributions from both mesodermal and neural crest ectodermal tissues. Key stages in its development occur between weeks 3 and 8 of gestation, marked by the formation of neural crest cells. These cells migrate and differentiate to form the carotid body, with growth factors such as nerve growth factor and brain-derived neurotrophic factor playing crucial roles in this process.
Transcription factors like Mash1 and Hoxa3 are essential for the formation and differentiation of carotid body cells during embryogenesis. Understanding the embryological development of the carotid body provides insights into its structure and function.
Developmental Timeline
The carotid body begins to form around the sixth week of gestation, with its cellular structures starting to differentiate. By the end of the first trimester, the carotid body exhibits a more organized structure with developing glomus cells.
During the second trimester, vascularization increases, enhancing the carotid body’s ability to sense oxygen levels. By the third trimester, the carotid body is functionally mature, ready to respond to fluctuations in blood chemistry at birth.
This timeline highlights the critical stages in the development of the carotid body, essential for its role in health.
Genetic Factors
Genetic factors play a crucial role in the development and functionality of the carotid body, influencing its structure and responses. Genetic anomalies can significantly impact the normal development and function of the carotid body, affecting its ability to react to physiological changes.
Understanding these genetic factors is essential for comprehending the overall role of the carotid body in human physiology and for developing targeted treatments for related disorders.
Surgical Considerations and Risks
Surgical procedures involving the carotid body require meticulous preoperative planning and careful postoperative care to minimize risks and ensure optimal outcomes. Preoperative planning may include imaging studies and embolization to reduce the risk of bleeding. Surgical risks associated with carotid body surgeries include cranial nerve injury and complications related to carotid body tumors.
Postoperative care is crucial for monitoring potential complications such as bleeding and nerve injuries, ensuring patient recovery. Understanding these considerations and risks is vital for the successful surgical management of carotid body conditions.
Preoperative Planning
Preoperative planning is critical in minimizing complications and ensuring optimal outcomes during surgeries involving the carotid body. Imaging tests are essential for assessing the anatomy of the carotid body and the presence of surrounding structures that may be affected during the procedure. For carotid body tumors, specific surgical strategies may be necessary due to their variable size, location, and vascularity.
Preoperative embolization can be performed to reduce vascularity and minimize bleeding risks during surgery. These steps are crucial for successful surgical interventions involving the carotid body.
Postoperative Care
Following surgery, it is crucial to closely monitor the patient in the recovery room to ensure they stabilize after anesthesia. Patients may require assistance from a caregiver post-surgery, especially if they experience limitations in mobility or daily activities.
Following postoperative care instructions from healthcare providers is essential to minimize the risk of complications and promote healing. Signs of potential complications, such as fever or increased pain at the surgical site, should prompt immediate consultation with a doctor.
Engaging in physical activity as advised can help prevent blood clots and maintain muscle strength. Proper postoperative care is vital for a smooth recovery and minimizing potential risks.
Carotid Body and Metabolic Disorders
The activity of the carotid body has been linked to the development of metabolic disorders, particularly in relation to obesity and insulin resistance. Overactivity of the carotid body can lead to increased sympathetic nerve activity, contributing to hypertension and other cardiovascular issues. Understanding the link between carotid body activity and metabolic dysfunctions provides insights into potential therapeutic targets for treating these conditions.
The following subsections will explore the effects of chronic intermittent hypoxia and potential therapeutic targets for metabolic disorders.
Chronic Intermittent Hypoxia
Chronic intermittent hypoxia (CIH) is a pathological condition that can significantly alter glucose homeostasis, leading to potential metabolic dysfunctions. CIH is associated with increased sympathetic nervous system activity, which can elevate blood pressure and heart rate. This heightened sympathetic tone can disrupt glucose metabolism and contribute to cardiovascular diseases.
The interplay between altered glucose homeostasis and increased sympathetic activity due to CIH is a critical factor in understanding the development of metabolic disorders. Addressing CIH is essential for managing its impact on cardiovascular and metabolic health.
Therapeutic Targets
The carotid body is implicated in various metabolic disorders, highlighting its role as a potential therapeutic target. Overactivity of the carotid body is associated with hypertension, which can exacerbate metabolic disorders and cardiovascular issues.
Targeting the carotid body to modulate its activity may offer new pharmacological strategies to mitigate conditions such as hypertension and obesity. Understanding these therapeutic targets is crucial for developing effective treatment options for metabolic disorders.