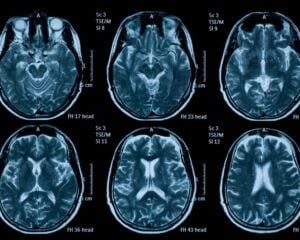
Brain parenchymal atrophy occurs when brain tissue shrinks and loses volume over time. This condition affects brain cells and their connections, leading to changes in memory, thinking, and movement. Recent studies show that approximately 46% of adults over 60 experience some degree of brain tissue loss, though the rate varies among individuals. Several factors can cause brain atrophy, including aging, head injuries, and various neurological diseases. Early detection through brain scans helps doctors create effective treatment plans and manage symptoms better.
Brain Parenchymal Structure
Your brain consists of an amazing structure called the parenchyma – the critical building block that makes all your thinking and movement possible. This remarkable tissue contains billions of nerve cells connected through an intricate network that works together seamlessly.
Parenchyma as a bustling city where neural cells live and communicate. These cells form the “gray matter” of your brain, packed with cell bodies and branch-like structures called dendrites. Each neural connection plays a specific role in helping you think, feel, and move.
The way these cells arrange themselves affects how well your brain works. A healthy brain parenchyma maintains dense, well-organized cellular networks. These networks process information rapidly and keep your cognitive abilities sharp.
Scientists study brain parenchyma patterns to spot early signs of neurological changes. By examining how cells connect and communicate, doctors can better help patients maintain optimal brain health. The more we learn about these incredible cellular communities, the better we become at protecting and supporting brain function.
Your brain’s parenchyma continues working round the clock, coordinating countless signals that make you uniquely you. This remarkable tissue demonstrates nature’s brilliant design in creating our most complex organ.
Primary Medical Conditions Linked to Atrophy
Brain parenchymal atrophy represents a critical neurological phenomenon observed across multiple progressive neurodegenerative disorders. Alzheimer’s Disease characteristically demonstrates significant cortical volume reduction, particularly in hippocampal and temporal regions.
Multiple Sclerosis manifests as widespread white matter atrophy and neuronal network disruption. Parkinson’s Disease further illustrates neurological degeneration through substantial subcortical gray matter loss, specifically impacting basal ganglia and substantia nigra structures.
Alzheimer’s Disease Impact
Alzheimer’s disease changes how the brain works in clear, measurable ways. Your brain cells gradually break down over time, causing memory problems and changes in how you think and function.
Picture your brain slowly losing its healthy tissue – this happens through damaged nerve cells and weakened connections between them. This damage shows up differently as the disease moves forward:
| Stage | Brain Changes | Daily Life Impact |
|---|---|---|
| Early | Small tissue loss | Forgetting recent events |
| Moderate | Noticeable shrinkage | Trouble with daily tasks |
| Advanced | Major tissue loss | Needs help with basic care |
| Terminal | Widespread damage | Requires full-time care |
The memory center of your brain, called the hippocampus, takes an especially hard hit. Brain scans show these areas getting smaller as nerve cells die off. Doctors track these changes through special brain imaging tests that reveal exactly where and how much damage has occurred.
This process affects real people in real ways. A person who once managed complex tasks now struggles with simple daily activities. A grandmother who told detailed stories now searches for basic words. These changes happen because specific parts of the brain stop working as they should.
Modern scanning technology helps doctors see these brain changes clearly. This gives families and caregivers a better picture of what’s happening and helps them plan appropriate care as symptoms progress.
Multiple Sclerosis Progression
Multiple sclerosis (MS) changes your brain in specific ways that doctors can now track and measure. The condition causes gradual damage to the protective coating around nerve cells, leading to brain tissue loss over time.
Brain scans show these changes happening in both the white and gray matter areas of your brain. Modern MRI technology helps doctors measure exactly where and how much tissue loss occurs each month or year. These detailed scans reveal changes in key brain regions, such as:
- The outer layer (cortex) that controls movement and thinking
- The hippocampus area involved in memory
- Deeper brain structures that coordinate various body functions
The ability to see these changes gives doctors valuable clues about how MS progresses in each person. This precise tracking helps them adjust treatments and manage symptoms more effectively.
Your doctor uses these brain measurements to:
- Monitor how active the MS remains
- Determine which treatments work best
- Track responses to different medications
- Plan ahead for potential challenges
Think of these scans as detailed maps showing exactly where MS affects your brain tissue. This helps create more targeted treatment plans focused on protecting the specific areas experiencing changes.
The process stays consistent – regular scans create a clear picture of tissue changes over time. This ongoing monitoring helps doctors stay ahead of potential problems and adjust care plans as needed.
These advanced imaging techniques continue improving our knowledge of MS patterns. They provide concrete data about brain changes, helping medical teams make better-informed decisions about your care.
Parkinson’s Neurological Degeneration
Parkinson’s disease affects the brain in specific ways that change how people move and feel. The condition damages certain brain areas, especially a region called the substantia nigra, which helps control movement.
Think of your brain’s movement control center as a complex network. In Parkinson’s, the cells that make dopamine – a crucial brain chemical – start to break down. This causes the familiar tremors and movement difficulties many patients experience.
Your medical team can help manage these changes through:
- Medications that boost dopamine levels
- Physical therapy exercises to maintain strength
- Regular movement practice for better balance
Brain Changes in Parkinson’s Disease
| What Changes | How It Affects You |
|---|---|
| Movement Control | Tremors and stiffness |
| Brain Chemistry | Less dopamine available |
The good news: many treatments work together to slow these changes. Your doctor creates a personal care plan that includes medications and exercises matched to your needs. Physical therapists teach specific movements to help maintain daily activities.
Brain-protective treatments target several goals:
- Preserving nerve cell function
- Maintaining brain connections
- Supporting daily activities
Medical teams customize these approaches based on each person’s symptoms. Regular check-ups help adjust treatments as needs change over time.
Small steps make big differences – from taking medications on schedule to practicing recommended exercises. Working closely with healthcare providers creates the best path forward for managing symptoms effectively.
Genetic and Hereditary Risk Factors
Your genes and family history shape your brain health in fascinating ways. Scientists have tracked specific changes in DNA that affect how brain cells work and survive. These genetic patterns run in families, creating complex networks that influence brain cell strength.
Think of genes like LRRK2, PARK7, and SNCA as key players in protecting your brain cells. Each one has a special role, much like different players on a sports team working together. Sometimes these genes change slightly, making brain cells more sensitive to damage over time.
The way your genes turn on and off adds another layer to this story. Picture your genes as light switches – some stay bright while others dim. Small chemical changes to your DNA, plus variations in your cell powerhouses (mitochondria), create unique patterns that affect brain health differently for each person.
Scientists study these patterns to develop better treatments that target specific genetic changes. Your genetic makeup acts like a roadmap, helping doctors choose the most effective ways to support your brain health. The more we learn about these genetic connections, the better we become at protecting brain cells and keeping them healthy longer.
Clinical Assessment and Neurological Evaluation
Clinical assessment of brain parenchymal atrophy requires a thorough neurological examination that systematically evaluates motor function, reflexes, sensory responses, and coordination.
Cognitive function testing employs standardized neuropsychological assessments to quantify potential deficits in memory, executive function, language processing, and visuospatial skills. These evaluative methods provide critical insights into the neurological manifestations and progression of parenchymal atrophy, enabling clinicians to characterize functional impairments and develop targeted intervention strategies.
Physical Neurological Examination
A neurological examination helps doctors check how well your brain and nerves work together. Your doctor acts like a detective, looking for clues about your nervous system’s health through specific tests and observations.
During the exam, your doctor checks several key areas of nerve function. They test your reflexes with a small rubber hammer and evaluate how you feel different sensations on your skin. They also watch how you move, balance, and coordinate your movements.
The doctor pays close attention to your cranial nerves – these control your face, eyes, hearing, and other functions in your head. They’ll ask you to follow their finger with your eyes or smile to test these nerves.
Your muscle strength gets tested too. The doctor asks you to push against their hands or lift your arms and legs. They check your muscle tone by moving your joints and feeling how your muscles respond.
Each finding gets carefully recorded. Your doctor compares these results with future exams to track any changes in your nervous system. This helps them spot problems early and create the right treatment plan for you.
The exam includes several hands-on tests:
- Tapping your knees to check reflexes
- Touching your skin with soft and sharp objects
- Walking heel-to-toe to test balance
- Moving your fingers to check coordination
- Testing muscle strength in arms and legs
These specific tests tell your doctor exactly how your nervous system performs its daily tasks. They show whether signals travel correctly between your brain and body parts.
Cognitive Function Testing
Doctors can measure your brain function with remarkable precision using specialized tests. These tests check different mental abilities like memory, problem-solving, speaking, and visual skills.
The Montreal Cognitive Assessment (MoCA) and Mini-Mental State Examination (MMSE) give doctors clear scores of your memory and thinking abilities. These tools help track small changes in brain function that regular check-ups miss.
Your doctor compares your test results with other people your age to spot any unusual changes. This creates a detailed picture of how your brain works across different areas. The tests feel like solving puzzles or answering questions about everyday things.
Each test focuses on specific mental skills. For example, you’ll draw shapes, remember word lists, or solve simple math problems. Your doctor guides you through each task while taking careful notes about your responses.
The results help create your personal brain health profile. This baseline shows your natural strengths and helps catch any future changes early. Your doctor uses this information to give you the right support and care based on your unique needs.
These cognitive tests give both you and your doctor valuable insights. They take the guesswork out of brain health by providing clear, measurable results. This helps everyone make better decisions about your care moving forward.
Current Treatment and Management Strategies
Your doctor creates a personalized treatment plan that targets the specific causes of brain tissue loss while protecting remaining brain cells. The plan combines medications, daily habits, and regular check-ups to help maintain brain health and daily functioning.
Medical teams work together to provide complete care that fits your needs. This includes brain-protecting medications along with exercises for both mind and body. A nutritionist helps plan brain-healthy meals, while physical therapists teach movements that keep you steady and strong.
Every few months, your doctor will check your memory, thinking, and physical abilities. These check-ups help track how well treatments work and guide any needed changes to your care plan. The main goal focuses on helping you stay independent and active while slowing down changes in your brain.
Your care team creates clear steps for managing symptoms at home and during medical visits. They teach practical ways to handle daily tasks and suggest tools that make activities easier. Regular exercise classes, memory training, and support groups add extra benefits to your medical treatment.
Small positive changes in diet, sleep, and daily routines can make a big difference. Your doctor will explain how each part of your treatment works and answer questions about managing symptoms. This team approach keeps you feeling supported while working toward better brain health.