If you’re on cholesterol medication and drink alcohol, you might wonder how to protect your liver. We’ll explain how these medications interact with alcohol, the risks involved, and how to minimize them. You’ll also learn about safe drinking limits and other medications that could be easier on your liver.
Key Takeaways
- Statins are essential for cholesterol management but can pose risks to liver health, especially when combined with heavy alcohol consumption.
- Routine monitoring of liver enzymes is crucial for individuals on statins, particularly if they consume alcohol, to catch potential liver issues early.
- Moderate alcohol intake (up to two drinks per day for men and one for women) is deemed safe for individuals on statins, but exceeding these limits can lead to serious health risks.
Cholesterol and Liver Health
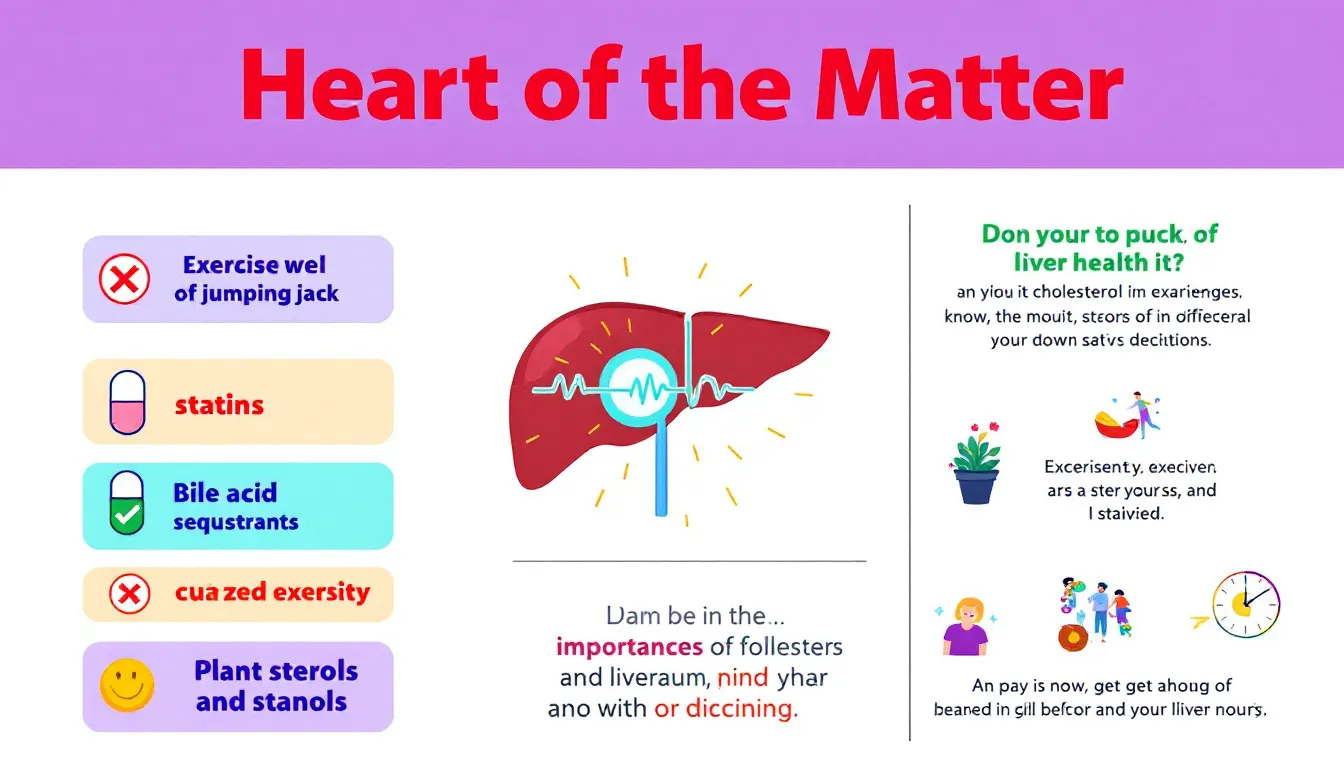
Statins are a cornerstone in managing high cholesterol and protecting heart health. Over 92 million adults in the U.S. alone are prescribed these medications for taking statins to keep cholesterol levels and total cholesterol level in check. One statin medicine works by blocking the enzyme necessary for cholesterol production in the liver, which effectively reduces LDL cholesterol, often referred to as “bad cholesterol.” Additionally, statins can increase high density lipoprotein cholesterol, the “good cholesterol,” which helps eliminate cholesterol from the body.
Long-term use of statins is often necessary to maintain lower cholesterol levels. However, they come with their own set of side effects. While muscle pain and muscle injury are common complaints, liver damage, although rare, can occur. For years, regular liver function tests were recommended to monitor statin-related myopathy and liver damage, but due to the low risk, this practice is no longer as common.
Cholesterol medications are generally safe for individuals with mild liver disease. However, heavy drinking can counteract the benefits of statins, potentially leading to higher cholesterol levels and increased cardiovascular risks. It’s worth noting that cholesterol-lowering medications like statins have an excellent safety record, with very little evidence of liver damage.
Understanding how these medicines work and their impact on liver health is crucial, especially when considering the effects of alcohol consumption.
Alcohol Consumption and Liver Function

Alcohol’s effect on liver function is a matter of significant concern. Excessive alcohol consumption can lead to liver damage, increasing the risk of side effects from statin medications. Long-term alcohol consumption is linked to liver diseases like nonalcoholic fatty liver disease (NAFLD) and chronic hepatitis, both of which can severely impact cholesterol metabolism and the effectiveness of cholesterol medications.
Heavy drinking can lead to fat accumulation in liver cells, a condition known as hepatic steatosis, which interferes with cholesterol metabolism. Over time, this can result in liver inflammation, scarring, and ultimately liver failure. Limiting alcohol intake is crucial, as excessive consumption not only damages liver cells but can also lead to severe conditions like liver cirrhosis and liver cancer.
For those on statins, the higher risk is even higher. The liver metabolizes both alcohol and statins, meaning heavy drinking can exacerbate liver problems and hinder the processing of these medications, leading to an increased risk of underlying liver disease and pre existing liver disease when you drink alcohol.
Disclaimer : Without Doctor consult , you can’t take it and first talk with your doctor first.
Statins and Alcohol: What You Need to Know
Combining statin therapy with alcohol consumption requires careful balance. Alcohol intake can elevate liver enzyme levels, complicating the assessment of liver health for those on cholesterol medications. Heavy drinking, in particular, can increase the risk of liver damage and liver toxicity.
Individuals with a history of liver damage should inform their doctors if they consume alcohol use, as it may affect their treatment plan. Moderate alcohol intake, defined as up to two drinks per day for men and one for women, is considered safe. However, exceeding these limits, or consuming more than two drinks, can lead to elevated triglyceride levels, worsened muscle side effects, and potential liver injury.
Monitoring alcohol consumption is crucial for those on statins. Heavy drinking combined with statin use may negate the drug’s benefits and amplify its side effects, posing significant health risks, including high risk. Additionally, the statins mix may further complicate these issues.
Monitoring Liver Enzymes While Drinking Alcohol
Ongoing liver function routine monitoring is crucial for those on statin therapy, particularly if they consume alcohol. A liver panel, including tests for key enzymes like alanine aminotransferase (ALT), often detects liver damage before symptoms appear. Regular liver tests can help ensure that any potential liver issues are caught early, allowing for timely intervention in a histopathological follow up study.
If minor elevations in liver enzyme levels are noted during statin use, continuing the medication is generally recommended rather than stopping it abruptly, as the benefits of statins often outweigh the clinically significant risks of elevated liver enzymes.
However, individuals should be cautious about consuming substances that may further stress the liver, such as too much grapefruit juice, which can interact with statins and affect liver function. Monitoring liver enzymes and being mindful of alcohol and other dietary interactions are key to managing overall health.
Safe Drinking Guidelines for Those on Statins
For individuals on cholesterol medications, limiting alcohol daily intake is crucial to avoid negative interactions and exacerbating liver issues. The recommended safe limit is one drink per day for women and two drinks per day for men. Moderating or eliminating alcohol intake is advisable for those on statins to minimize the risk of liver damage and ensure the medication’s effectiveness.
Discussing personal alcohol limits with a healthcare provider is crucial for those on statins. A personalized approach can balance the benefits of statin therapy with the upper limit of risks of alcohol consumption, ensuring optimal health outcomes.
Lifestyle Changes to Support Liver Health
Supporting liver health goes beyond medication. A balanced diet rich in fresh fruits, vegetables, whole grains, and healthy fats can significantly improve liver function. Maintaining a healthy weight is crucial to preventing fatty liver disease, which can result from obesity or being overweight. Regular exercise helps reduce liver fat and aids in burning excess triglycerides.
Avoiding exposure to household toxins and chemicals can protect liver cells from damage. Staying hydrated supports overall liver function. These lifestyle changes, combined with careful monitoring of alcohol intake, help ensure your liver remains healthy while on cholesterol medications.
Consulting Your Healthcare Provider
Open communication with healthcare providers is crucial for those on statin therapy who consume alcohol and may have various risk factors. Patients should discuss their alcohol consumption openly to create a personalized treatment strategy. Sometimes providers may hesitate to address alcohol misuse due to discomfort or fear of damaging the patient-provider relationship, but clear communication is vital for effective advice and support.
It’s also important for patients to disclose all medication use, including over-the-counter and herbal products, as well as other medicines, to their healthcare provider. This ensures potential drug interactions are identified, allowing for adjustments to the treatment plan.
Summary
In summary, while statins are highly effective in managing high cholesterol and protecting heart health, their interaction with alcohol requires careful consideration. Limiting alcohol intake, monitoring liver enzymes, and consulting healthcare providers are essential steps in ensuring the safe and effective use of cholesterol medications.
By understanding the benefits and risks of combining statins with alcohol, and exploring alternative medications and lifestyle changes, individuals can make informed decisions that support both their liver and heart health.
Frequently Asked Questions
Can I drink alcohol while taking statins?
Yes, moderate alcohol consumption is generally safe while taking statins, but heavy drinking can increase the risk of liver damage and other side effects. It is important to monitor your alcohol intake to avoid potential health risks.
How often should I monitor my liver enzymes if I drink alcohol while on statins?
It is advisable to monitor liver enzymes regularly if consuming alcohol while on statins to identify any potential liver problems early. This proactive approach ensures your liver health is managed effectively.
Are there cholesterol medications with fewer liver risks than statins?
Yes, alternatives such as ezetimibe, bempedoic acid, and PCSK9 inhibitors are associated with fewer liver risks compared to statins. These options can be considered for patients concerned about liver health.
What lifestyle changes can support my liver health while on statins?
To enhance liver health while on statins, it is crucial to adopt a balanced diet, engage in regular exercise, maintain a healthy weight, avoid toxins, and ensure adequate hydration. These lifestyle changes will significantly contribute to your overall liver well-being.
Should I discuss my alcohol consumption with my healthcare provider?
Yes, you should discuss your alcohol consumption with your healthcare provider, as open communication enables the development of a personalized treatment plan that addresses both the benefits and risks associated with your health.