Did you know that both hydrocephalus and ventriculomegaly involve an excess of cerebrospinal fluid, but they represent different concerns? It’s crucial to understand how each condition affects the brain, especially in the case that you or someone you know is facing these diagnoses. While hydrocephalus can lead to serious complications and requires careful management, ventriculomegaly often resolves with little intervention. Let’s investigate the key differences that could assist you in better grasping these terms and their implications.
Definition and Overview
Hydrocephalus and ventriculomegaly could sound similar, but they represent different conditions involving cerebrospinal fluid in the brain.
Ventriculomegaly refers to the enlargement of the lateral ventricles due to an accumulation of cerebrospinal fluid (CSF). You may see this condition on a prenatal ultrasound as soon as the lateral ventricles measure more than 10 mm.
In many cases, ventriculomegaly can resolve on its own, leading to a favorable prognosis with a 90% chance of normal development.
On the other hand, hydrocephalus involves a more significant accumulation of fluid, often due to aqueductal stenosis or other blockages. Hydrocephalus can lead to increased intracranial pressure and is associated with neurodevelopmental delays, requiring ongoing management to prevent complications.
Causes and Risk Factors
In recognizing hydrocephalus and ventriculomegaly, it’s crucial to acknowledge the role of both genetic factors and environmental influences.
Genetic conditions can elevate the risk of these conditions, while factors like maternal infections during pregnancy can greatly affect brain development.
Through exploring these causes and risk factors, you’ll gain a clearer depiction of how they influence individuals differently.
Genetic Factors
Genetic factors play a significant role in the development of hydrocephalus, adding complexity to this condition. Conditions like X-linked hydrocephalus arise from mutations, such as those in the L1CAM gene, affecting approximately 1 in 30,000 births. About 7% of male hydrocephalus cases link to genetic conditions like Bickers-Adam syndrome. Chromosomal abnormalities on various chromosomes also increase risk. Familial cases often show a genetic predisposition, revealing family histories of similar conditions. Associated abnormalities, such as spina bifida or agenesis of the corpus callosum, further enhance the chances of both hydrocephalus and ventriculomegaly.
| Genetic Factor | Associated Conditions | Impact |
|---|---|---|
| Mutations in L1CAM | X-linked hydrocephalus | Affects 1 in 30,000 births |
| Chromosomal abnormalities | Various recognized chromosomes | Increases risk of hydrocephalus |
| Familial cases | Family history of conditions | Suggests genetic predisposition |
| Associated abnormalities | Spina bifida, ACC | Raises risk of hydrocephalus and ventriculomegaly |
Environmental Influences
Anyone preparing for parenthood should be aware that various environmental factors can greatly influence fetal development, particularly concerning conditions like hydrocephalus and ventriculomegaly.
Maternal infections, such as cytomegalovirus and syphilis, pose risks through the potential to lead to these conditions. Exposure to teratogenic substances, including certain medications and drugs, can result in congenital brain anomalies impacting cerebrospinal fluid (CSF) flow.
Additionally, should you be older, increased maternal age can raise the chance of chromosomal disorders that could cause ventriculomegaly and hydrocephalus.
Genetic factors also play a role, interacting with environmental influences. For instance, mutations related to hydrocephalus may be compounded by prenatal maternal health conditions.
Being informed helps one take proactive steps for a healthy pregnancy.
Symptoms and Clinical Presentation
Hydrocephalus and ventriculomegaly can seem similar at first glance, but their symptoms and clinical presentations highlight important differences that can significantly impact diagnosis and treatment.
In hydrocephalus, you might notice symptoms associated with increased intracranial pressure, such as an enlarged head size, bulging fontanelle, irritability, and vomiting.
In contrast, many cases of ventriculomegaly show no symptoms during pregnancy and are often identified later. However, severe ventriculomegaly can lead to symptoms like poor feeding and muscle tone abnormalities.
The clinical presentation of hydrocephalus is often evident sooner, while ventriculomegaly may not show immediate signs until postnatal assessment.
Acknowledging these differences is vital for ensuring timely diagnoses and appropriate management strategies.
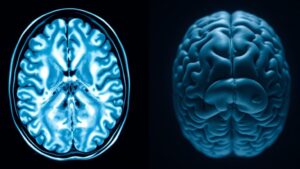
Diagnostic Methods and Imaging Techniques
Upon the matter of diagnosing conditions like hydrocephalus and ventriculomegaly, healthcare providers depend on various imaging techniques that can offer essential insights into a baby’s brain development.
For detecting ventriculomegaly, a prenatal ultrasound is typically the initial step, with a measurement of the lateral ventricles exceeding 10 mm indicating potential issues. Fetal MRI can complement ultrasounds, providing a closer look at areas that might be unclear.
After birth, further imaging, including ultrasounds or MRIs, helps confirm the diagnosis, evaluating for hydrocephalus and the condition of the cerebrospinal fluid (CSF).
Through distinguishing between mild, moderate, and severe ventriculomegaly, providers can tailor management strategies effectively, keeping your baby’s neurodevelopmental health a priority.
Treatment and Management Strategies
As it pertains to managing ventriculomegaly and hydrocephalus, tackling the unique needs of each child becomes a top priority for healthcare providers.
- Treatment for ventriculomegaly usually involves careful monitoring after birth, intervening only in severe cases.
- Hydrocephalus management often requires a ventriculoperitoneal shunt to relieve pressure from cerebrospinal fluid.
- Fetal monitoring through serial ultrasounds helps track progress and defines the need for interventions when ventricular enlargement worsens.
- In specific cases, endoscopic third ventriculostomy might be the preferred alternative to shunt surgery.
Post-operative care and regular follow-ups are essential for both conditions, ensuring that any complications are addressed promptly.
This attentive management approach helps secure the best results for your child.
Prognosis and Developmental Outcomes
While a diagnosis of ventriculomegaly or hydrocephalus can feel overwhelming, it’s important to recall that the prognosis varies greatly depending on the specific circumstances of each case.
For instance, isolated mild ventriculomegaly often has favorable results, with just a 0% to 8% chance of developmental abnormalities. In contrast, severe ventriculomegaly, which indicates hydrocephalus, raises concerns, as about 60% of infants might face neurodevelopmental delays.
Regular monitoring is vital for tracking developmental progress. Approximately half of the infants with isolated hydrocephalus can achieve normal results, but the presence of other brain anomalies can complicate the situation.
Ultimately, comprehending the subtleties of each diagnosis can guide you in seeking appropriate support and interventions.
Support Services and Resources
Comprehending that your child faces a diagnosis of hydrocephalus or ventriculomegaly can feel overwhelming, but many resources are available to guide your family through this process.
Here are some key support services to weigh:
- The Richard D. Wood Jr. Center offers access to healthcare professionals who can provide guidance and information.
- Neurosurgery departments facilitate surgical treatment, including shunt placements, as part of a coordinated approach.
- The Neonatal Neurocritical Care Program provides specialized post-delivery care for infants, managing potential complications effectively.
- The division of neurology can help you comprehend fetal neurological conditions and guarantee appropriate consultations for specific needs.
Embracing these resources can lead you to a supportive community that will help steer through this experience.