Lower leg redness might indicate infections, blood clots, or other serious conditions. Quick identification and treatment are crucial. This article covers the causes, symptoms, and treatments of lower leg redness to help you manage the condition effectively.
Key Takeaways
- Lower leg redness can signal serious conditions such as infections, blood clots, or venous insufficiency, making early recognition vital for effective treatment.
- Common symptoms include swelling, pain, warmth, skin changes, and itching, which can help identify underlying causes and necessitate medical evaluation.
- Preventive measures like regular exercise, good hygiene, proper footwear, and managing risk factors are essential for reducing the occurrence of lower leg redness.
Lower Leg Redness
Lower leg redness can indicate underlying issues like infections, blood clots, or venous insufficiency. Paying attention to changes in your lower limbs allows for early detection, significantly improving treatment outcomes.
Regular exercise improves blood circulation, which can help prevent lower leg redness. Staying vigilant and proactive helps you maintain leg health effectively.
Causes of Lower Leg Redness
Various causes can lead to lower leg redness, such as infections, blood clots, and venous insufficiency. Each cause has its own symptoms and risk factors, so identifying the specific reason behind the redness is important.
Infections like cellulitis, for instance, can lead to significant swelling and pain. Blood clots, on the other hand, might present similar symptoms but require different treatment approaches. Identifying these causes allows for tailored treatments and helps avoid potential complications.
Infections
Infections often cause lower leg redness.
Cellulitis, a bacterial skin infection, frequently affects the lower limbs of the body, often due to skin breaks from conditions like athlete’s foot and recurrent cellulitis, as well as from issues related to feet, including staphylococcus aureus.
Fungal infections can also cause redness.
Cellulitis symptoms include:
- pain
- warmth
- swelling
- significant redness.
Individuals with chronic edema are especially prone to cellulitis, as bacteria thrive in swollen areas. Blood tests may be required to rule out other infections and assess inflammatory markers.
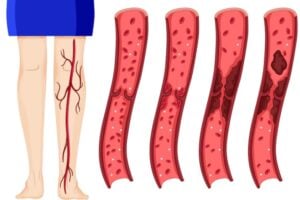
Blood Clots
Blood clots, especially deep vein thrombosis (DVT), can cause lower leg redness and are often mistaken for cellulitis due to similar symptoms. Ultrasounds are frequently used to detect clots by evaluating blood flow and identifying blockages in the leg veins.
Prompt diagnosis and treatment are crucial, as untreated blood clot can lead to serious complications like pulmonary embolism. Recognizing the signs and risk factors of blood clots ensures timely medical intervention.
Venous Insufficiency
Venous insufficiency happens when the valves in the leg veins malfunction, causing blood to pool. This leads to symptoms like heaviness, pain, and redness. Varicose veins, a common manifestation, can cause chronic symptoms, including redness and swelling around the ankles and lower calves.
Skin changes, such as tan or reddish-brown discoloration, may occur and are often exacerbated by conditions like varicose eczema. Untreated varicose veins can result in significant skin discoloration and complications like venous eczema and venous stasis eczema dermatitis.
Allergic Reactions
Allergic reactions can cause lower leg redness. Common allergens include certain foods, medications, and insect bite. Symptoms range from mild redness and itching to severe swelling and discomfort. Identifying and avoiding allergens helps prevent reactions.
Over-the-counter antihistamines and topical creams can manage symptoms, but severe reactions might require medical attention.
Skin Conditions
Various skin conditions can cause lower leg redness. Psoriasis, for example, results in red, scaly patches that can be painful and itchy. Rosacea, primarily affecting the face, can also extend to the legs, causing redness and swelling.
Managing these conditions involves ongoing management, topical treatments, lifestyle changes, and sometimes systemic medications to reduce inflammation and redness.
Symptoms Associated with Lower Leg Redness
Lower leg redness often accompanies symptoms like swelling, warmth, pain, skin changes, and itching. These signs can indicate underlying conditions needing medical attention.
Recognizing the full spectrum of symptoms aids in identifying the root cause and seeking appropriate treatment for full recovery.
1. Swelling
Swelling commonly accompanies lower leg redness and can result from fluid retention, venous stasis, or heart-related issues. This swelling can pressure the skin, causing discomfort and changes in skin color. Persistent swelling may lead to skin irritation or ulcers if not addressed.
Deep vein thrombosis or heart failure can also cause significant swelling in the lower legs.
2. Warmth or Heat in the Affected Area
Increased warmth in the affected area is a common symptom of lower leg redness, indicating inflammation or infection. Conditions like cellulitis cause pain and tenderness, making the infected skin feel warmer than the surrounding area.
Warmth often accompanies increased swelling, signaling that medical evaluation might be necessary.
3. Pain and Tenderness
Pain and tenderness are significant indicators of lower leg redness, often stemming from blood vessel problems or infections. Conditions like cellulitis make the affected area red, warm, and extremely painful.
Severe pain with redness might indicate a serious condition requiring prompt medical evaluation to ensure it is treated quickly.
4. Skin Changes (Blisters, Ulcers)
Skin changes like blisters or ulcers can result from prolonged swelling or poor circulation. Conditions like cellulitis or venous stasis dermatitis may cause significant damaged skin alterations related to various health conditions, including other complications, skin problems, and skin condition.
Leg ulcers, often found between the knee and ankle, might ooze fluid if untreated and can vary in color from red to purple or yellow. These issues require careful monitoring and treatment to prevent complications.
5. Itching or Rashes
Itching or rashes on the legs can result from skin inflammation or allergies. Dermatitis, including varicose eczema, often appears as red, itchy patches on the lower leg. Contact dermatitis can stem from reactions to irritants, causing rashes or inflammation.
Treatment usually involves avoiding irritants and using anti-inflammatory creams to reduce itching, which can be effectively treated. This approach can also serve as a way to treat the underlying issues.
Diagnosing Lower Leg Redness
Proper diagnosis of lower leg redness is crucial for effective treatment. Identifying the underlying cause allows for a tailored approach to manage the condition. If cellulitis is suspected, contacting a GP promptly ensures quick and effective treatment, preventing complications.
Medical Examination
During a medical examination for lower leg redness, a healthcare provider will assess the condition visually and ask relevant questions about symptoms and medical history. This helps determine the cause of the redness and any further diagnostic steps needed.
Understanding the patient’s history and symptoms is key for a correct diagnosis and effective treatment.
Further Tests
Further tests may be conducted to accurately diagnose lower leg redness. Tests like the ankle brachial pressure index (ABPI) assess blood flow and compression stocking suitability. Blood tests and temperature checks can confirm a cellulitis diagnosis.
Referral to a vascular specialist or dermatologist may be necessary for additional tests related to lower leg conditions.
Treatment Options for Lower Leg Redness
Treatment for lower leg redness aims to halt skin damage progression and reduce flare-ups or complications. Neglected venous disease can worsen skin discoloration and cause pain and hardness. Proper treatment helps prevent permanent redness.
Exploring various treatment options ensures the right approach for each specific cause of lower leg redness.
Antibiotic Therapy
Antibiotic therapy is necessary if a bacterial infection causes lower leg redness. Completing the entire course of antibiotics ensures effective treatment. In cellulitis with lymphoedema, the antibiotic regimen may be longer than usual.
Sometimes, a second or extended antibiotic course is required to ensure the infection has completely cleared.
Compression Stockings
Compression stockings are designed to support veins and improve blood flow in the legs. They apply graduated compression to prevent blood pooling and reduce symptoms of venous insufficiency.
Wear compression stockings to effectively manage lower leg redness and associated symptoms.
Pain Management
Pain management is crucial for treating lower leg redness. Over-the-counter medications like ibuprofen or acetaminophen can reduce pain and swelling. Home remedies like elevating the leg, applying cold compresses, or soaking the leg in Epsom salt also help manage pain and reduce swelling.
Combining these methods offers comprehensive pain relief for those experiencing lower leg redness.
Preventing Lower Leg Redness
Preventing lower leg redness involves adopting lifestyle changes and skincare practices. Here are some effective strategies:
1. Good Hygiene Practices
Proper hygiene is crucial for preventing skin infections and lower leg redness. Clean, dry skin reduces fungal growth risk, while regularly changing clothes and bed linens minimizes moisture accumulation, preventing infections.
Using personal towels and not sharing personal items significantly lowers the infection spread risk. Thoroughly drying the skin after showering or bathing, especially in moisture-prone areas, further reduces the risk of infections leading to lower leg redness.
2. Wearing Proper Footwear
Choosing high-quality, well-fitting shoes prevents discomfort and inflammation in the legs. Comfortable footwear supports proper posture and reduces leg stress during walking or standing. Shoes with good arch support alleviate strain and minimize swelling risk.
Avoiding tight or restrictive shoes enhances blood circulation in the lower legs and reduces irritation risk. Breathable materials and supportive shoes minimize heat buildup and skin inflammation.
3. Avoiding Long Periods of Standing or Sitting
Prolonged sitting or standing can lead to fluid accumulation in the legs, causing swelling. Regular movement is essential to prevent swelling in the lower extremities. Elevating the legs elevated can help reduce swelling if you’ve been sitting or standing for too long.
Engaging in short walks and changing positions regularly can mitigate swelling and improve circulation in the legs. Elevating the legs above heart level during rest promotes better blood flow and helps reduce swelling.
4. Regular Exercise
Engaging in regular physical activity enhances blood circulation, which can help mitigate swelling and redness in the legs. Low-impact exercises, such as walking or swimming, are particularly beneficial for individuals experiencing leg swelling, as they promote fluid movement without placing stress on the joints.
Resistance training strengthens leg muscles, playing a crucial role in fluid movement and reducing symptoms related to leg swelling. High-intensity interval training (HIIT) can improve cardiovascular health and enhance the lymphatic system flow, potentially lowering the risk of swelling in the lower legs.
5. Skin Care Tips
Regularly applying sunscreen can prevent skin damage and redness caused by sun exposure. Using a fragrance-free moisturizer on the legs can help protect against skin irritation and redness. Keeping an eye on any existing wounds or blisters is crucial for preventing infections that can lead to redness.
Maintaining proper skin care is vital in preventing lower leg redness and potential infections. Regularly moisturizing dry skin helps prevent fissures and other skin issues that might cause inflammation or redness.
6. Managing Risk Factors
Managing risk factors for lower leg redness involves taking proactive steps to reduce the likelihood of recurrence. Swollen legs due to a damaged lymph system can increase the likelihood of cellulitis. Existing skin conditions are risk factors for recurrence of cellulitis in lymphoedema. Good skin care and avoiding breaks in the skin help prevent recurrent episodes of cellulitis.
Moisturizing with an unperfumed moisturizer and monitoring blisters and wounds are essential practices for caring for legs affected by lower leg redness.
When to Seek Medical Attention
It’s important to know when to seek medical attention for lower leg redness. If swelling in the leg is severe or appears suddenly without an obvious cause, urgent medical help should be sought. Redness or heat in the swollen area, along with high fever, indicates the need for immediate medical attention.
Persistent swelling that does not improve after a few days of home treatment warrants a visit to a healthcare provider. People with diabetes experiencing leg swelling should consult a doctor promptly. Starting antibiotics immediately and seeking medical opinion if familiar symptoms of cellulitis develop is crucial.