Pancreatitis after gallbladder removal, though uncommon, can be a significant concern for some patients, occurring in about 5% of cases, particularly within the initial year. This condition often stems from complications like retained gallstones, bile duct injuries, or sphincter of Oddi dysfunction, which disrupt normal digestion.
Symptoms such as severe abdominal pain, nausea, or jaundice can mimic other post-surgical issues, making diagnosis tricky. Comprehending the risks and causes is key to addressing this condition effectively and easing recovery. What happens next can make all the difference.
Incidence of Pancreatitis Post-Cholecystectomy
How often does pancreatitis occur after gallbladder removal? Approximately 5% of patients develop pancreatitis following cholecystectomy, the medical term for gallbladder removal surgery. The risk is highest in the initial year after the procedure, with an incidence ranging from 2-4%. Certain groups, such as aged patients and those with a history of gallstone-related acute pancreatitis, face a greater likelihood of this complication.
Retained or recurrent gallstones, bile duct injury, and sphincter of Oddi dysfunction are common causes of postcholecystectomy pancreatitis. Symptoms like abdominal pain, nausea, and diarrhea, often associated with postcholecystectomy syndrome, can sometimes mimic pancreatitis, making diagnosis more complex. Comprehending the incidence and risk factors helps patients and healthcare providers monitor for potential complications after gallbladder surgery. Prompt detection can improve outcomes and guarantee timely treatment.
Causes of Pancreatitis After Gallbladder Removal
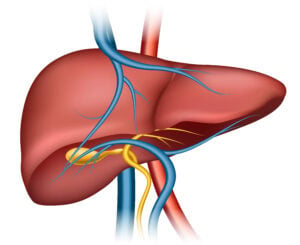
Although gallbladder removal, or cholecystectomy, is often a straightforward procedure, it can occasionally lead to pancreatitis—a painful and concerning complication. One common cause is bile duct stones, which can migrate and obstruct the pancreatic duct, leading to inflammation. Bile reflux into the pancreatic duct, often due to bile duct injuries or leaks, can also trigger pancreatitis. Postcholecystectomy syndrome, characterized by symptoms like biliary colic, might sometimes involve complications that affect the pancreas. Additionally, dysfunction of the sphincter of Oddi, the muscle controlling bile and pancreatic juice flow, can cause pancreatic duct obstruction. Anatomical variations in the common bile duct or pancreatic duct further increase the risk.
| Cause | Mechanism |
|---|---|
| Bile duct stones | Obstruct pancreatic duct |
| Bile reflux | Inflames pancreatic tissue |
| Sphincter of Oddi dysfunction | Disrupts bile and pancreatic juice flow |
| Anatomical variations | Increase duct obstruction risk |
Retained Stones in the Bile Duct
Retained stones in the bile duct are a significant concern after gallbladder removal, affecting 5-15% of patients and often leading to pancreatitis. These stones, also known as common bile duct stones, can remain undetected during surgery or form afterward, causing blockages that trigger inflammation of the pancreas.
Inadequate surgical exploration or missed stones during initial imaging are common reasons for their persistence. Postoperative imaging and careful intraoperative examination are essential to identify and prevent such complications.
If retained stones are diagnosed, endoscopic retrograde cholangiopancreatography (ERCP) is frequently used to remove them, alleviating symptoms and reducing the risk of pancreatitis. Awareness of this issue helps patients and healthcare providers address it promptly, ensuring better recovery and minimizing long-term complications.
Surgical Injury to the Biliary Tract
Surgical injury to the biliary tract, while uncommon, is a serious complication that can occur during gallbladder removal surgery. Bile duct injuries, such as bile leaks or bile duct strictures, can disrupt normal bile flow, leading to bile duct obstruction or bile accumulation in the abdomen.
These injuries can result from anatomical variations, adhesions, or technical challenges during cholecystectomy. Symptoms often include abdominal pain, fever, and jaundice, signaling a need for prompt evaluation.
Endoscopic retrograde cholangiopancreatography (ERCP) is commonly used to diagnose and manage these issues, such as sealing bile leaks or dilating strictures. For severe biliary tract injuries, surgical repair may be necessary to restore proper anatomy and prevent long-term complications. Timely detection and treatment are crucial for optimal recovery.
Mimics of Post-Cholecystectomy Pancreatitis
Post-cholecystectomy pancreatitis can be challenging to distinguish from other conditions, such as biliary tract disorders, sphincter of Oddi dysfunction, or peptic ulcer disease. Each of these mimics could present with symptoms like abdominal pain, nausea, or elevated liver enzymes, requiring careful evaluation.
Accurate diagnosis through imaging or endoscopic techniques is critical to guarantee suitable treatment and prevent unwarranted interventions.
Biliary Tract Disorders
Several conditions affecting the biliary tract can mimic the symptoms of pancreatitis after gallbladder removal, making it challenging to pinpoint the exact cause of discomfort. Biliary disease, such as bile duct obstruction due to stones, can disrupt bile flow and cause pain similar to pancreatic issues.
Patients could experience upper abdominal pain, nausea, or jaundice, which are common in both conditions. Bile duct inflammation or infection, known as cholangitis, can also simulate pancreatitis by causing severe pain and fever. Additionally, residual or migrated stones in the bile duct after gallbladder removal can lead to blockages, further complicating diagnosis.
These biliary tract disorders necessitate careful evaluation through imaging and blood tests to differentiate them from pancreatic inflammation and guarantee proper treatment.
Sphincter of Oddi Dysfunction
Sphincter of Oddi dysfunction is a condition that can cause significant discomfort after gallbladder removal, affecting up to 15% of patients who’ve undergone the procedure. It occurs when the sphincter of Oddi, a muscle regulating bile and pancreatic ducts, malfunctions due to dyskinesia (abnormal movement) or stenosis (narrowing). This dysfunction can lead to recurrent abdominal pain, mimicking pancreatitis, as increased pressure builds in the ducts. Diagnosis often involves endoscopic retrograde cholangiopancreatography (ERCP) with manometry to measure sphincter pressure. Addressing this condition might include medications like smooth muscle relaxants, endoscopic sphincterotomy, or surgery to relieve the obstruction. Comprehending this condition is essential for differentiating it from other post-cholecystectomy complications.
| Key Aspect | Details |
|---|---|
| Cause | Dyskinesia or stenosis of sphincter of Oddi |
| Symptoms | Recurrent abdominal pain, pancreatitis-like |
| Diagnosis | ERCP with manometry |
| Treatment | Medications, endoscopic sphincterotomy, surgery |
| Incidence | Up to 15% post-cholecystectomy patients |
Peptic Ulcer Disease
- Endoscopy is the definitive diagnostic tool, allowing doctors to witness ulcers clearly.
- Proton pump inhibitors and H2 receptor antagonists are primary treatments to reduce symptoms.
- If symptoms linger despite acid suppression therapy, further tests could eliminate other causes.
- Neglected ulcers can deteriorate, so prompt diagnosis and treatment are vital.
Distinguishing between peptic ulcers and pancreatitis guarantees proper care and relief for patients.
Diagnostic Approaches for Post-Cholecystectomy Pancreatitis
Diagnosing post-cholecystectomy pancreatitis begins with identifying clinical symptoms such as persistent abdominal pain, nausea, or vomiting. Laboratory testing, including serum amylase and lipase levels, provides initial confirmation of pancreatic inflammation.
Advanced imaging techniques like CT, MRI, or endoscopic ultrasound help assess the extent of pancreatic damage and identify contributing factors.
Clinical Symptoms Identification
After gallbladder removal, some individuals could experience sudden and intense abdominal pain, often signaling post-cholecystectomy pancreatitis. This condition can mimic other issues like gallstone disease, postcholecystectomy syndrome (PCS), or even acute necrotizing pancreatitis. Recognizing these symptoms at an early stage is critical for effective treatment. Imaging studies and tests like a complete blood count (CBC) or endoscopic retrograde cholangiopancreatography (ERCP) may be necessary to confirm the diagnosis.
- Pain that radiates to the back—intense and unrelenting, making daily tasks unbearable.
- Nausea and vomiting—leaving patients feeling drained and helpless.
- Unexplained fever or chills—raising fears of infection or complications.
- Yellowing of the skin or eyes—signaling potential bile duct issues.
Understanding these signs can help individuals seek timely care, easing their recovery path.
Laboratory Testing Utilization
At a time that someone experiences abdominal pain after gallbladder removal, laboratory tests become an essential step in figuring out what’s going on. Blood tests are often the primary step to check for pancreatitis, focusing on serum amylase and lipase levels. Elevated levels, particularly amylase over 1000 IU/L, strongly suggest gallstone-induced or biliary pancreatitis. Liver function tests are also integral, as elevated ALT levels (over 3 times normal) can indicate bile duct issues. These tests help distinguish pancreatitis from other conditions. Combining these findings with imaging studies, such as ultrasound or MRI, helps pinpoint the cause.
| Test | Purpose |
|---|---|
| Amylase and Lipase | Confirm pancreatitis |
| Liver Function Tests | Identify bile duct obstruction |
| Blood Tests | General diagnostic assessment |
Imaging Techniques Application
Right after gallbladder removal, when abdominal pain persists, imaging techniques intervene to uncover the underlying cause. These procedures are vital for identifying complications such as acute pancreatitis or common bile duct stones, which can develop post-cholecystectomy.
Key imaging tools include:
- Ultrasound: Detects gallstones and biliary dilation, offering a quick and non-invasive first step in diagnosis.
- CT scanning: Highly accurate for confirming acute pancreatitis and assessing its gravity, especially with contrast-enhanced CT.
- Endoscopic ultrasound: Provides detailed imaging of the biliary tract, matching ERCP’s precision without invasive measures.
- MRCP: Near-equivalent to ERCP in identifying retained common bile duct stones, making it a safer alternative.
These methods guarantee precise diagnoses and guide effective treatment, helping patients navigate post-cholecystectomy complications with confidence.
Management and Prevention Strategies
Managing pancreatitis after gallbladder removal involves several strategies to reduce recurrence and prevent complications. Endoscopic retrograde cholangiopancreatography (ERCP) can help remove stones or debris blocking the bile ducts, while temporary stenting guarantees the pancreatic duct stays open, preserving pancreatic juice flow and preventing obstruction-induced pancreatitis.
Monitoring with a complete blood count (CBC) helps detect inflammation promptly. Postcholecystectomy syndrome (PCS), caused by a remnant cystic duct or bile flow issues, may necessitate surgical intervention. Preserving pancreatic acinar cells and preventing pancreatic duct ligation are key to reducing inflammation.
Combining endoscopic sphincterotomy with elective cholecystectomy significantly decreases recurrence rates. Avoiding triggers and maintaining bile flow are practical prevention steps. Prompt diagnosis and customized treatment plans guarantee better outcomes for patients.
Conclusion
Post-cholecystectomy pancreatitis, though uncommon, can be a serious complication, particularly in the initial year after surgery. Recognizing the causes, such as retained stones or bile duct injuries, and distinguishing it from mimics like peptic ulcers, is key to effective treatment. While some may worry about the risk being overstated, the 5% incidence highlights the need for awareness. Prompt diagnosis and tailored management substantially improve outcomes and reduce complications, ensuring smoother recovery for affected patients.