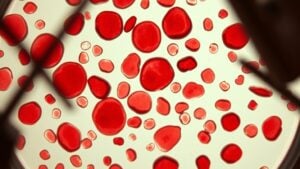
Envision your red blood cells as tiny delivery trucks transporting oxygen throughout your body. Whenever these trucks begin to take on unusual shapes, it’s known as poikilocytosis, and it can signal some vital fundamental health issues. You may notice symptoms like fatigue or shortness of breath, which can make everyday life challenging. Curious about what causes these changes and how to stay healthy? We should investigate the reasons behind poikilocytosis and what it means for your blood health.
What Is Poikilocytosis?
*When* you *contemplate* red blood cells, you likely *visualize* them as those perfect little biconcave disks, right? However, poikilocytosis flips the script, showing abnormally shaped red blood cells (RBCs) that take on odd forms like crescents, teardrops, or spikes.
This condition, marked by at least 10% abnormal red blood cells in your blood sample, isn’t a disease on its own but hints at fundamental issues affecting RBC production or function. Genetic disorders like sickle cell anemia, nutritional deficiencies, liver problems, or bone marrow abnormalities can be culprits.
To diagnose it, healthcare providers often perform a complete blood count and a blood smear test, analyzing peripheral blood to understand the various cell shapes and potential root causes.
What Are the Symptoms of Poikilocytosis?
As you consider poikilocytosis, you may observe some surprising symptoms. You could feel tired or weak, and shortness of breath may creep in as your body struggles to get enough oxygen.
While you pay attention to your body, look out for any signs of dizziness or changes in skin color, which can signal something’s not quite right.
Common Symptoms Overview
Provided you’ve been feeling more exhausted lately, it could be due to something more than just a busy schedule. Poikilocytosis can lead to several noticeable symptoms that impact your daily life. Here’s a quick overview:
| Symptom | Description | Cause |
|---|---|---|
| Fatigue | Constant tiredness | Reduced oxygen delivery |
| Weakness | Lack of physical strength | Dysfunctional RBCs |
| Shortness of Breath | Difficulty in breathing | Impaired oxygen transport |
You could also notice pale skin or jaundice as blood cell destruction occurs. Rapid heartbeat and dizziness are common too, as your body tries to compensate for low oxygen levels. Headaches often come with this too, signaling that your brain’s not getting enough oxygen.
Anemia-Related Signs
Grasping the symptoms related to poikilocytosis is crucial, particularly since they can often be confused for ordinary fatigue. Should you notice fatigue and weakness, it could stem from abnormally shaped red blood cells that aren’t supplying enough oxygen.
You may also observe pale or yellowish skin, especially should your poikilocytosis be due to hemolytic anemias or liver issues. Shortness of breath and dizziness might arise as your body isn’t getting enough oxygen, leading to a rapid heartbeat as your heart works harder to compensate.
In severe cases, untreated anemia might result in chest pain or even organ dysfunction. Being aware of these signs can help you seek the necessary medical attention promptly.
Severity and Variability
Symptoms of poikilocytosis can vary widely, and comprehending this range can assist you in identifying the moment to seek medical help. The presence of abnormally shaped RBCs can lead to mild fatigue or severe issues, depending on their percentage in your blood. For example, should over 30% of your RBCs be abnormal, you may experience chronic weakness and shortness of breath. Severe cases can cause jaundice or rapid heartbeat. Below is a brief overview of different symptoms related to various types of poikilocytes:
| Type of Poikilocyte | Associated Symptoms |
|---|---|
| Sickle Cells | Vaso-occlusive pain |
| Spherocytes | Hemolytic anemia |
| Eliptocytes | Weakness, fatigue |
| Acanthocytes | Jaundice, dizziness |
Understanding these symptoms can help you better manage your health!
What Causes Poikilocytosis?
You could be surprised to learn that poikilocytosis can come from both inherited conditions and various acquired factors.
Disorders like sickle cell disease and thalassemia create irregular red blood cells because of abnormal hemoglobin.
On the other hand, things like nutritional deficiencies, liver issues, and even alcohol abuse can disrupt your body’s ability to produce healthy red blood cells.
Inherited Conditions Impact
Inherited conditions can markedly influence the shape and function of red blood cells (RBCs), leading to a condition known as poikilocytosis. For instance, sickle cell anemia, caused by abnormal hemoglobin S, produces crescent-shaped RBCs and affects many individuals, particularly African-Americans.
Thalassemia creates target cells due to imbalanced globin chain production, impacting many worldwide. Hereditary spherocytosis results in spherical RBCs due to defective cytoskeleton proteins, mainly in people of Northern European descent.
Pyruvate kinase deficiency leads to irregularly shaped cells due to glycolysis issues, while McLeod syndrome, an X-linked genetic mutation, causes spiked RBCs. These inherited conditions remind us that our genetic makeup directly affects our blood health, so comprehending them is vital for managing your wellbeing.
Acquired Factors Influence
While genetic factors can play a major role in poikilocytosis, acquired conditions also heavily influence the shape and functionality of red blood cells. For instance, iron deficiency can greatly impair red blood cell production, leading to abnormal shapes.
Chronic alcoholism doesn’t just harm the liver; it also affects nutrient absorption, which can result in poikilocytosis. Liver disease, like cirrhosis, disrupts lipid metabolism, causing cells to assume irregular shapes, such as acanthocytes.
Kidney disease can alter electrolyte balance and lower erythropoietin production, impacting red blood cell health too. Additionally, malaria infections directly damage red blood cells, leading to fragmentation.
Grasping these acquired factors is essential for maintaining ideal blood health and tackling any fundamental issues.
What Are the Complications of Poikilocytosis?
At the time you experience severe poikilocytosis, the consequences can go far beyond what you could anticipate. Chronic oxygen deprivation can lead to organ damage, particularly affecting your heart and brain. Should it remain untreated, you could encounter life-threatening anemia, with hemoglobin levels dropping dangerously low.
Those with sickle cell-related poikilocytosis are at risk for vaso-occlusive crises, causing excruciating pain and tissue ischemia. Liver disease-associated poikilocytosis could advance to hepatic failure unless addressed appropriately.
Additionally, hereditary spherocytosis can cause splenomegaly and gallstones, which might require surgical intervention in many cases. Identifying these complications is vital for taking proactive steps in your health path.
How Is Poikilocytosis Diagnosed?
When you suspect poikilocytosis, your doctor will likely start with a peripheral blood smear test to look at your red blood cells under a microscope.
They’ll also perform a complete blood count to check the size of your cells and hemoglobin levels, giving them a clearer understanding of your condition.
In case needed, they’ll order additional tests to rule out nutritional deficiencies or other fundamental health issues.
Blood Smear Examination
A precise diagnosis of poikilocytosis often begins with a simple yet revealing blood smear evaluation. During a blood smear test, a thin layer of blood is spread on a slide and stained, allowing you to inspect different RBC shapes under a microscope.
Medical technologists look for abnormal shapes, like spherocytes and sickle cells, in a peripheral blood smear. Should you have 10% or more of these irregular RBCs, it could suggest poikilocytosis.
This test often accompanies a complete blood count to provide more background. Should unusual RBC morphology be found, your doctor could propose additional iron studies or genetic testing to reveal the root cause, helping guide your treatment.
Complete Blood Count
Grasping how poikilocytosis is diagnosed involves assessing your Complete Blood Count (CBC), which contains crucial details about your general health. A CBC measures your red blood cells (RBCs), hemoglobin, hematocrit, and other key indices.
Should your test show low hemoglobin or hematocrit, it could indicate anemia and raise a red flag for poikilocytosis. An increased Red Cell Distribution Width (RDW) suggests a variation in the size and shape of your RBCs.
Should abnormalities appear, your doctor could recommend a blood smear to closely inspect your cells. They may also propose iron studies to find the root cause.
Keep in mind, monitoring your blood health is a key part of your total wellness path!
Additional Diagnostic Tests
To diagnose poikilocytosis effectively, healthcare providers often recommend a series of additional diagnostic tests that provide a clearer representation of your blood health. These tests help pinpoint the exact cause behind the abnormal red blood cells.
| Test Type | Purpose |
|---|---|
| Complete Blood Count (CBC) | Measures hemoglobin levels, RBC count, and indices. |
| Peripheral Blood Smear (PBS) | Identifies specific types of poikilocytes. |
| Serum Iron, Ferritin, | Assesses for iron deficiency as a potential cause. |
| Transferrin Saturation | |
| Vitamin B12 and Folate Levels | Rules out megaloblastic anemia. |
| Liver Function Tests (LFTs) | Checks for liver disease. |
| Kidney Function Tests | Evaluates kidney health in case organ disease is suspected. |
These tests help healthcare providers create a comprehensive view of your health. Keep in mind, grasping your results is key!
How Is Poikilocytosis Treated?
How can poikilocytosis be effectively treated? The key is tackling the root cause. For instance, if you have iron-deficiency anemia, iron supplements can enhance your red blood cell (RBC) production. Vitamin B12 shots could be useful for pernicious anemia.
In hereditary issues like sickle cell disease, doctors often prescribe hydroxyurea to improve RBC function. If your symptoms are severe, you may need blood transfusions to restore RBC levels and relieve fatigue.
Autoimmune-related poikilocytosis can benefit from immunosuppressive therapies or corticosteroids to minimize RBC destruction. In rare situations, such as hereditary spherocytosis, a splenectomy could be recommended to prevent excessive breakdown of your RBCs.
Each option focuses on improving your general blood health and wellness.
What Is the Outlook for Individuals With Poikilocytosis?
Understanding the outlook for individuals with poikilocytosis often depends on identifying the fundamental causes and managing them effectively. Should you be handling iron deficiency, timely discovery and intervention can result in a normal life expectancy and complete recovery.
For those with inherited conditions like sickle cell disease or thalassemia, lifelong care could be required, but many live into their 50s or beyond with contemporary treatments. Nevertheless, severe cases stemming from bone marrow disorders or advanced liver disease may have worse prognoses without measures such as transplants.
Routine monitoring is vital for those with genetic forms, as unmanaged complications can greatly influence long-term results. Resolving fundamental causes swiftly can make a notable difference in your outlook.
Can Poikilocytosis Be Prevented?
Can you really take steps to prevent poikilocytosis? Absolutely! Start through maintaining a balanced diet rich in iron, vitamin B12, and folate. This helps keep iron deficiency at bay and supports blood health.
Regular blood tests can catch initial signs of issues, ensuring you stay ahead of potential problems. Limiting alcohol consumption is also key; it reduces your risk of liver disease and nutrient malabsorption, both linked to poikilocytosis.
Provided you have chronic conditions, managing them with prescribed treatments helps lower your risk, too. Finally, consider genetic counseling provided there are inherited causes of poikilocytosis in your family.
Timely identification allows for better management, so you can focus on staying healthy and feeling your best!
When Should I See My Healthcare Provider?
Taking care of your health is a top priority, particularly when you’re aware of the risk factors for poikilocytosis. If you’re experiencing persistent fatigue, weakness, or shortness of breath, it’s vital to see your healthcare provider, as these symptoms could indicate anemia related to poikilocytosis.
Notice pale or yellowish skin? That might signal abnormal red blood cell function, so don’t hesitate to consult a professional. Rapid or irregular heartbeat can reflect severe anemia too.
Should you have a family history of inherited blood disorders like sickle cell disease or thalassemia, reach out for a risk assessment. Finally, in case blood tests show over 10% poikilocytes, it’s time to investigate the root causes with your healthcare provider.
Is Poikilocytosis Serious?
Comprehending the seriousness of poikilocytosis can feel overwhelming, especially as you weigh the root causes that could drive it. This condition can indicate foundational conditions, such as sickle cell disease or myelofibrosis, which could lead to serious complications.
The percentage of abnormal red blood cells plays a vital role in severity. For instance, untreated cases could progress to organ damage or heart failure. With certain genetic disorders, you may even face a reduced life expectancy should you not seek timely treatment for poikilocytosis.
However, initial diagnosis and tackling factors like iron deficiency can help make it less serious. Always discuss your symptoms with your healthcare provider so you can investigate appropriate diagnosis or treatment options together.