Spinal cord injuries disrupt the signals between the brain and body, often causing paralysis and loss of sensation. What causes these injuries? How can you identify them? And what are the best treatment options? In this article, we answer these crucial questions to help you understand spinal cord injuries better.
Key Takeaways
- Spinal cord injuries are categorized into complete and incomplete types, with the severity and location of the injury significantly impacting motor and sensory function.
- Common causes of spinal cord injuries include traumatic events like motor vehicle accidents and falls, as well as non-traumatic conditions such as degenerative diseases and congenital factors.
- Effective management of spinal cord injuries requires a multidisciplinary rehabilitation approach, addressing physical, emotional, and social aspects of recovery while also exploring innovative treatments like stem cell therapy.
Spinal Cord Injuries
A spinal cord injury is defined as damage to the spinal cord that results in a loss of function, such as mobility or sensation. The spinal cord itself is a complex bundle of nerves that relay messages between the brain and the rest of the body, playing a critical role in our bodily functions. When this delicate structure is compromised, the consequences can be profound, affecting both motor and sensory function capabilities below the spinal injury site.
Spinal cord injuries are categorized into two main types: complete and incomplete. A complete injury means there is no communication between the brain and parts of the body below the injury, resulting in total loss of sensory and motor function. In contrast, an incomplete injury retains some degree of communication, allowing for partial sensory or motor function below the injury site. The location of the injury also plays a crucial role in determining the extent of the disability. For instance, injuries to the upper spinal cord (cervical spinal cord) can lead to tetraplegia, affecting all four limbs, while injuries lower down may result in paraplegia, impacting only the legs.
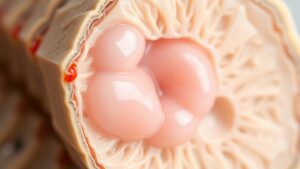
The spinal cord is composed of nerve cells, fibers, and blood vessels, all of which are essential for its function. At the lower end, structures like the conus medullaris and cauda equina are vital for various bodily functions. Understanding these components and their interactions helps grasp the full impact of spinal cord damage.
Conditions like Brown-Séquard syndrome, where injury on one side of the spinal cord leads to unique patterns of motor and sensory loss, further illustrate the complexity of spinal cord injuries.
Common Causes of Spinal Cord Injuries
Spinal cord injuries can result from a variety of causes, broadly categorized into traumatic and non-traumatic origins. Traumatic spinal cord injuries are often sudden and violent, resulting from incidents like motor vehicle accidents, falls, and sports injuries. On the other hand, non-traumatic causes include medical conditions such as degenerative diseases, infections, and tumors. Understanding these causes is essential for both prevention and treatment.
In addition to these broad categories, specific medical conditions and congenital factors can also lead to spinal cord injuries. Conditions like multiple sclerosis and spinal stenosis, as well as congenital issues like spina bifida, are significant contributors. Exploring these causes provides a comprehensive understanding of spinal cord injuries and their management.
1. Traumatic Causes
Traumatic spinal cord injuries are the result of sudden, forceful impacts or penetrations that damage the spinal cord. Motor vehicle accidents are the leading cause, accounting for over 31% of spinal cord injuries, particularly among younger individuals. These accidents often result in severe spinal cord trauma and are a major focus of prevention efforts where spinal cord injuries occur.
Falls are another significant cause, especially among older adults aged 76 and above, who are more prone to slipping and falling. Sports injuries, particularly from high-impact sports like football and diving, also contribute to a substantial number of cases of sports related injuries.
Violence, including gunshot wounds and stab wounds, represents approximately 12% of spinal cord injuries and disproportionately affects younger individuals. Workplace accidents, often involving falls or hazardous conditions, are another cause of traumatic spinal cord injuries. Risk factors such as age, alcohol use, and lack of protective gear further increase the likelihood of these injuries.
2. Non-Traumatic Causes
Non-traumatic spinal cord injuries result from medical conditions that gradually damage the spinal cord. Degenerative diseases like osteoarthritis can cause spinal stenosis, leading to compression and injury to the spinal cord. Infections, such as meningitis or abscesses, can also lead to spinal cord damage if not promptly treated.
Tumors, whether benign or malignant, can grow within or near the spinal cord, causing pressure and injury. Strokes and spinal cord vascular malformations are other non-traumatic causes that can lead to significant spinal cord damage.
Early diagnosis and intervention are crucial to prevent severe outcomes in these conditions.
3. Medical Conditions Leading to Spinal Cord Injuries
Several medical conditions can predispose individuals to spinal cord injuries. Multiple sclerosis, for example, is an autoimmune disease that attacks the protective covering of nerve fibers, leading to spinal cord damage. Spinal stenosis, characterized by the narrowing of the spinal canal, can compress the spinal cord and nerves, causing injury.
Syringomyelia, a condition where cysts form within the spinal cord, can lead to significant neurological disorders. Transverse myelitis, an inflammatory disorder affecting the spinal cord, and other autoimmune diseases are additional medical conditions that can result in spinal cord injuries.
These conditions underscore the complex interplay between various medical factors and spinal cord health.
4. Congenital Causes
Congenital causes of spinal cord injuries are present from birth and result from developmental anomalies. Spina bifida, a condition where the spinal column does not close completely, exposes the spinal cord and nerves to damage. Chiari malformation, where brain tissue extends into the spinal canal, can also lead to spinal cord compression and injury.
Congenital spinal deformities, such as scoliosis or kyphosis, can exert abnormal pressure on the spinal cord, leading to injury over time. Early detection and intervention in these congenital conditions can prevent long-term complications.
Symptoms of Spinal Cord Injuries
The symptoms of spinal cord injuries can vary widely depending on the severity and location of the injury. Common symptoms include severe back pain, weakness, numbness, and loss of bladder or bowel control. Prompt medical attention is needed as these symptoms can significantly impact an individual’s quality of life.
The severity of symptoms is often evaluated based on the loss of sensation and motor control below the injury site. Spinal cord injuries can result in paraplegia, affecting the lower half of the body, or quadriplegia, affecting all four limbs. A neck injury can have widespread effects, impacting not only the same areas as chest and lower back injuries but also the arms and breathing.
The neurological level of the injury indicates the lowest part of the spinal cord that remains undamaged.
1. Loss of Motor Function
Loss of motor function is a primary symptom of spinal cord injuries. This can range from partial paralysis to complete paralysis, depending on the severity of the injury. Tetraplegia, or quadriplegia, results in paralysis from the neck down, affecting all four limbs and the torso. Paraplegia, on the other hand, affects only the lower half of the body, impacting the legs and pelvic organs.
This loss of motor function can significantly alter a person’s ability to perform daily activities.
2. Sensory Impairment
Sensory impairment is another significant symptom of spinal cord injuries. Individuals may experience a loss of sensation, including numbness, tingling, or a complete absence of touch sensation. Neuropathic pain, a burning or sharp pain resulting from nerve pain, is also common.
Additionally, some individuals may lose the ability to perceive temperature changes, which can have increased risk safety implications.
3. Autonomic Dysfunction
Autonomic dysfunction occurs when the injury affects the autonomic nervous system, which controls involuntary bodily functions. This can lead to difficulties in breathing or other respiratory problems. Loss of bladder and bowel control is another common issue, significantly impacting daily life and social interactions.
Sexual dysfunction and abnormal blood pressure regulation, such as hypotension or hypertension, are additional symptoms of sexual functioning and autonomic dysfunction.
4. Reflex Impairments
Reflex impairments are also common in spinal cord injury patients. Hyperreflexia, or exaggerated reflexes, can occur, leading to muscle spasms and involuntary movements. Spasticity, characterized by muscle tightness or stiffness, and clonus, repeated uncontrolled muscle spasms, are other reflex impairments that can affect mobility and comfort.
5. Other Symptoms
Other symptoms of spinal cord injuries include loss of coordination (ataxia), muscle weakness, and difficulty swallowing (dysphagia). These symptoms can further complicate the recovery process and require targeted therapeutic interventions to manage effectively.
Severity of Spinal Cord Injuries
The severity of spinal cord injuries is a critical factor in determining the appropriate treatment and rehabilitation strategies. Injuries are classified based on the completeness of the injury and the neurological level affected. This classification significantly impacts the rehabilitation approach and the potential for recovery.
In addition to the complete and incomplete classifications, the level of injury—whether cervical, thoracic, lumbar spine, lumbar vertebra, or sacral—plays a crucial role in the overall impact on the patient. Understanding these classifications helps in tailoring the most effective treatment plans.
1. Complete Spinal Cord Injury
A complete spinal cord injury results in a total loss of sensory and motor function below the injury site. This means all communication between the brain and the body parts below the injury is lost, leading to significant and permanent impairment.
Rehabilitation strategies for complete injuries focus on maximizing independence and quality of life.
2. Incomplete Spinal Cord Injury
In an incomplete spinal cord injury, there is partial preservation of sensory or motor function below the injury site. Different syndromes characterize these injuries, such as Anterior Cord Syndrome, Brown-Séquard Syndrome, and Central Cord Syndrome.
Each type of incomplete injury presents unique challenges and requires specific rehabilitation strategies to optimize recovery and function.
3. Level of Injury
The level of injury on the spinal cord significantly affects the outcomes and rehabilitation process. Cervical injuries often result in quadriplegia, affecting all limbs and potentially respiratory function. Thoracic injuries typically lead to paraplegia, impairing trunk and lower limb function. Lumbar and sacral injuries impact the lower limbs and pelvic organs, but some trunk function may remain intact.
The ASIA Impairment Scale is commonly used to assess the severity across different levels.
Immediate Response to Spinal Cord Injuries
Immediate response to a suspected spinal cord injury is crucial to prevent further damage and complications. Promptly calling for emergency medical help is crucial. Emergency responders use precautions such as neck collars and backboards to immobilize the patient and prevent additional injury from a back or neck injury. Heavy towels or rolled sheets can also be placed alongside the neck to restrict movement.
In cases where there is no breathing or pulse, CPR should be initiated without moving the head. Rolling an injured person should involve a coordinated effort to maintain spinal alignment.
In the emergency room, sensory and movement tests help rule out spinal cord injuries. These immediate actions stabilize the patient and prevent secondary injury.
Diagnosing Spinal Cord Injuries
Diagnosing spinal cord injuries involves a combination of clinical examinations, diagnostic testing, and imaging studies. Neurological assessments are crucial for promptly evaluating symptoms and determining the extent of the injury. X-rays are used to identify damage to the bony structures surrounding the spinal cord.
CT scans provide detailed cross-sectional images, helping visualize bone and disc abnormalities. MRI scans are essential for detecting herniated discs or blood clots that may be affecting the spinal cord. Early diagnosis is crucial for effective treatment and significantly impacts recovery outcomes.
Treatment Options for Spinal Cord Injuries
The primary goals of spinal cord injury treatment are to prevent further injury and promote an active recovery. Surgery may be necessary to remove bone fragments or herniated disks compressing the spinal cord. Medications help manage pain, muscle spasticity, and improve bladder and bowel control. Spinal cord injuries treated effectively can lead to better outcomes for patients.
Newer treatment methods focus on enhancing neural regeneration through techniques like neuroplasticity and cell-based therapies. Neural stem cells are considered one of the most promising methods for promoting recovery following spinal cord injuries. Traction may be used to stabilize the spine and restore proper alignment.
These treatments aim to maximize functional recovery and enhance the quality of life for spinal cord injury patients.
Complications Associated with Spinal Cord Injuries
Spinal cord injuries often lead to a range of complications that require careful management. Urinary tract infections are common due to bladder dysfunction, necessitating effective management strategies to prevent infections. Pressure sores are also a significant risk due to impaired sensation and mobility. These sores can sometimes require surgical intervention if they become severe.
Deep vein thrombosis (DVT) can occur due to immobility, increasing the risk of blood clots in the limbs. Autonomic dysreflexia, a condition seen in individuals with injuries at T6 or higher, can cause dangerous spikes in blood pressure. Preventive measures for DVT include the use of anticoagulants, promoting physical activity, and strategies to relieve pressure, which can help prevent a blood clot.
Addressing these complications improves the overall health and well-being of spinal cord injury patients.
Rehabilitation and Recovery
Rehabilitation is a critical component of the recovery process for spinal cord injury patients. A comprehensive rehabilitation program involves a multidisciplinary team, including physiatrists, physical and occupational therapists, and psychologists. Physical therapy focuses on exercises that help maintain muscle strength and prevent contractures. Occupational therapy helps patients regain their roles in society and manage daily activities effectively.
Innovative medical devices, such as advanced wheelchairs and electrical stimulation systems, are being developed to enhance mobility and independence. Individuals with spinal cord injuries are prone to chronic complications that can diminish their functional independence and quality of life. Spinal cord injury rehabilitation addresses these challenges and improves the overall well-being of spinal cord injury patients through the use of assistive devices.
Advances in Spinal Cord Injury Research
Significant advances in spinal cord injury research are providing new hope for patients. Researchers are focusing on nerve regeneration and reducing inflammation after an injury to enhance recovery outcomes. Therapeutic research primarily focuses on neuroprotection. It also focuses on neuroregeneration.
Tissue engineering is being explored to rebuild damaged tissues in spinal cord injuries. Stem cell therapy is a novel intervention that holds promise for spinal cord injury patients, although it is still under investigation.
These innovative methods aim to enhance recovery outcomes and potentially restore function for individuals with spinal cord injuries.
Living with a Spinal Cord Injury
Living with a spinal cord injury presents numerous challenges, but with the right support and resources, individuals can lead fulfilling lives. Education about spinal cord injuries empowers individuals to contribute effectively to advocacy efforts. Emotional support from family, friends, and caregivers helps manage daily challenges. Peer support networks provide valuable information and emotional support, helping individuals cope with the challenges of living with a spinal cord injury.
Bowel and bladder dysfunction can significantly alter social relationships and activities. Accepted and proactive planning are strategies employed by individuals to cope with these effects, including bladder control. Community involvement plays a significant role in providing emotional and practical support to those living with spinal cord injuries.
Chronic pain management and diet are also crucial aspects of living with a spinal cord injury.
How You Can Help Improve SCI Care
There are several ways you can help improve spinal cord injury (SCI) care. Participation in clinical trials is vital as it contributes to advancing SCI treatments and improving care. Supporting SCI research can lead to breakthroughs that improve the quality of life for individuals affected by spinal cord injuries.
Advocating for better resources and care for SCI patients is crucial for fostering community awareness and support. Community involvement and support are essential for improving SCI care and ensuring patients receive the attention and resources they need. By getting involved, you can make a significant impact on the lives of those affected by spinal cord injuries.
Frequently Asked Questions
What are the main causes of spinal cord injuries?
The primary causes of spinal cord injuries are traumatic events such as motor vehicle accidents, falls, sports injuries, and violence, alongside non-traumatic factors like degenerative diseases, infections, tumors, and congenital conditions. Understanding these causes is crucial for prevention and awareness.
What are the symptoms of a spinal cord injury?
Spinal cord injuries can manifest as severe back pain, weakness, numbness, loss of bladder or bowel control, and sensory impairments. It is crucial to seek immediate medical attention if these symptoms arise.
How are spinal cord injuries diagnosed?
Spinal cord injuries are diagnosed through clinical examinations, neurological assessments, and imaging studies such as X-rays, CT scans, and MRIs, which help evaluate the injury’s extent and detect any associated damage. This thorough approach is crucial for effective management and treatment planning.
What treatment options are available for spinal cord injuries?
Various treatment options for spinal cord injuries encompass surgical interventions, pain management medications, neural regeneration methods, physical therapy, and advanced medical devices aimed at improving mobility and independence. These approaches collectively work to enhance patient outcomes and quality of life.
How can I help improve spinal cord injury care?
You can significantly enhance spinal cord injury care by participating in clinical trials, advocating for improved resources, supporting research efforts, and engaging in community initiatives that focus on improving the quality of life for those affected. Your involvement can make a meaningful difference.