Bone marrow is the spongy tissue inside bones that produces blood cells. Understanding bone marrow is crucial because it affects blood cell production and immune health. In this guide, we’ll explore its functions, types, and implications for health and disease.
Key Takeaways
- Bone marrow is a crucial organ responsible for producing nearly all blood cells and plays a significant role in supporting the immune system.
- There are two types of bone marrow: red marrow, which produces blood cells, and yellow marrow, which stores fat and can convert back to red marrow in emergencies.
- Maintaining healthy bone marrow involves a balanced diet, avoiding toxins, and regular medical check-ups to detect potential disorders early.
What is Bone Marrow
Bone marrow is the spongy tissue found within the cavities of our bones. It is a major hematopoietic organ, responsible for producing nearly all the blood cells in our body, including red blood cells, white blood cells, and platelets. The bone marrow consists of various cell types, including sympathetic nerves, Schwann cells, adipocytes, osteoblasts, osteocytes, and fibroblasts, each playing a crucial role in regulating and organizing hematopoiesis.
Recognizing disease alterations and designing efficient blood cell production systems rely on understanding the organization of the bone marrow.
Types of Bone Marrow
There are two main types of bone marrow: red marrow and yellow marrow. Red bone marrow is responsible for producing blood stem cells, which can develop into various blood cells, including red blood cells, white blood cells, and platelets. This type of marrow is found mainly in flat bones such as the pelvis, sternum, and the cavities of long bones in children. Red bone marrow remains red throughout life due to its role in hematopoiesis.
On the other hand, yellow bone marrow predominantly consists of fat and contains stem cells that have the potential to transform into cartilage, fat, or bone cells. As we age, some of the red bone marrow is gradually replaced by yellow marrow, which is mainly found in the central cavities of long bones.
Although yellow bone marrow is less active in hematopoiesis, it can revert to red marrow if necessary, such as in cases of severe blood loss or anemia.
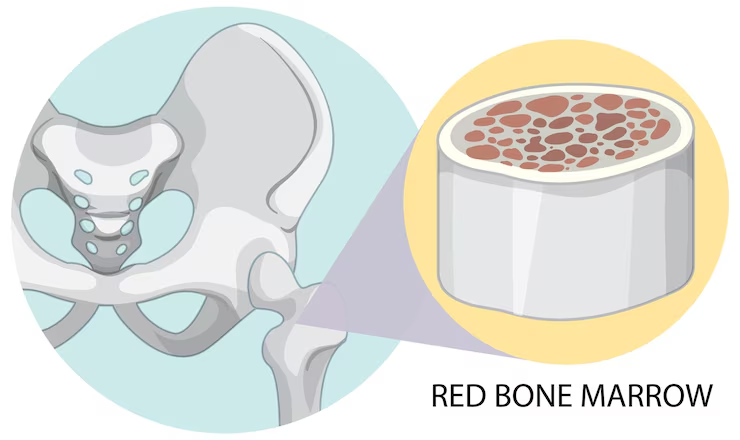
Red Bone Marrow
The red bone marrow houses hematopoietic stem cells that differentiate into various blood cells, making it a powerhouse of blood cell production. Located in the flat bones and at the ends of long bones, it is especially rich in stem cells and progenitor cells that initiate blood cell production. The red bone marrow is crucial for erythropoiesis (formation of red blood cells), leukopoiesis (formation of white blood cells), and thrombopoiesis (formation of platelets).
This type of bone marrow also plays a significant role in supporting the immune system by producing lymphocytes, which are key components of the immune response. The environment within the red bone marrow, known as the bone marrow niche, provides the necessary support and signals for stem cells to proliferate and differentiate into mature blood cells.
This process ensures a steady supply of new blood cells, crucial for maintaining overall health and fighting infections.
Diagram of Red Bone Marrow
Yellow Bone Marrow
Yellow bone marrow is primarily composed of adipocytes (fat cells) and serves as a storage site for fats, which can be utilized as an energy reserve. It contains mesenchymal stem cells that have the potential to differentiate into various cell types, including bone, cartilage, and fat cells. This type of marrow is found in the central cavities of long bones and becomes more prevalent with age as it gradually replaces red bone marrow.
Although less active in blood cell production compared to red marrow, yellow bone marrow plays a vital role in maintaining the body’s energy balance and supporting bone structure.
In certain conditions, such as severe anemia or blood loss, yellow marrow can convert back to red marrow to boost blood cell production. This adaptability allows the body to respond to increased demands for blood cells when needed.
Diagram of Yellow Bone Marrow
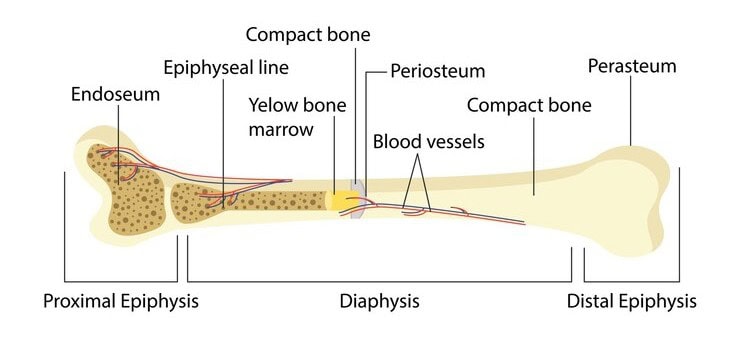
Structure of Bone Marrow
The structure of bone marrow is a complex and well-organized system situated within the cavities of bones, characterized by a rich supply of blood vessels and extensive nerve innervation. This spongy tissue is composed of a combination of hematopoietic cells, fat cells, and supportive stromal cells, creating an environment that is crucial for the production and maturation of blood cells.
The intricate architecture of the bone marrow ensures harmonious function to support hematopoiesis and maintain overall health.
Cellular Components
The cellular components of bone marrow stem cells include a variety of cells that play essential roles in hematopoiesis. Hematopoietic stem cells are the cornerstone of this process, giving rise to all types of blood cells. These stem cells differentiate into progenitor cells, which further mature into specific blood cell types such as red blood cells, white blood cells, and platelets.
Stromal cells in the bone marrow, including fibroblasts, endothelial cells, and adipocytes, provide structural and functional support to the hematopoietic cells. These marrow stromal cells are involved in producing colony-stimulating factors, which are crucial for the proliferation and differentiation of hematopoietic cells.
The interaction between hematopoietic and stromal cells within the bone marrow is crucial for maintaining a healthy and productive environment.
Non-Cellular Components
In addition to its cellular components, bone marrow contains several non-cellular elements that are essential for its function. The extracellular matrix offers structural support and plays a key role in cell signaling and hematopoiesis. This matrix is composed of proteins and other molecules that create a scaffold for the cells, helping to maintain the integrity of the bone marrow tissue.
Blood vessels and nerves are also integral parts of the bone marrow structure. The rich network of blood vessels facilitates the transport of nutrients and the exit of mature blood cells into circulation. These vessels ensure the bone marrow receives the oxygen and nutrients necessary for cell production and function. Additionally, the presence of nerves helps regulate the bone marrow’s activities and responses to the body’s needs.
Functions of Bone Marrow
Bone marrow is a critical organ for the production of nearly all blood components, including red blood cells, white blood cells, and platelets. Its functions extend beyond hematopoiesis, playing a vital role in supporting the immune system and maintaining the bone marrow microenvironment.
These functions are essential for overall health and the body’s ability to meet physiological demands and challenges.
Hematopoiesis (Blood Cell Production)
Hematopoiesis is the bone marrow’s process of producing new blood cells. This process is essential for maintaining a steady supply of red blood cells, white blood cells, and platelets, which are crucial for transporting oxygen, fighting infections, and preventing bleeding, respectively. Red bone marrow is the primary site for hematopoiesis, where hematopoietic stem cells differentiate into various blood cell types.
Erythropoiesis, the formation of red blood cells, ensures that our body has enough cells to carry oxygen from the lungs to tissues. Leukopoiesis, which involves the production of white blood cells, is vital for our immune response. Thrombopoiesis, the creation of platelets, helps prevent excessive bleeding by facilitating blood clotting. These processes underscore the importance of healthy red bone marrow for sustaining life.
Bone marrow diseases can impair blood production, leading to health complications like anemia, increased infection risk, and bleeding disorders. Conditions like leukemia can cause the bone marrow to produce large quantities of immature white blood cells, disrupting the balance of blood cell production. Maintaining healthy bone marrow is essential for efficient hematopoiesis and overall well-being.
Immune System Support
Bone marrow plays a vital role in supporting the immune system by producing lymphocytes, which are key components of the immune response. Lymphocytes include B cells that create antibodies and T cells that regulate immune responses and attack infected or cancerous cells.
Bone marrow facilitates antigen presentation, where immune cells display pathogen pieces to T cells, initiating an immune response. This interaction between bone marrow cells and the immune system is crucial for maintaining health and protecting the body against infections and diseases. A healthy bone marrow is therefore essential for a robust and effective immune system.
Bone Marrow Microenvironment
The bone marrow microenvironment includes specialized structures like sinusoids, arterioles, and endosteal surfaces, crucial for hematopoiesis. These structures form distinct niches that provide support and regulate the growth and differentiation of hematopoietic stem cells. These niches ensure that immature blood cells undergo various stages of development before becoming fully functional mature blood cells.
Spatially organized microenvironments within the bone marrow regulate unique aspects of hematopoiesis, essential for blood cell production. For instance, certain regions are specialized for the maintenance of hematopoietic stem cells, while others support the differentiation of specific blood cell types. This complex organization is vital for producing a diverse and functional array of blood cells needed for various bodily functions.
Hematopoietic Stem Cells
Hematopoietic stem cells (HSCs) are critical for generating different types of blood cells throughout an individual’s life. These stem cells reside in the bone marrow and have the unique ability to self-renew and differentiate into various blood cell lineages, including red blood cells, white blood cells, and platelets.
The continuous production and regulation of these cells are crucial for a healthy and functional hematopoietic system.
Blood Cell Production
Blood cell production, or hematopoiesis, primarily occurs in the red bone marrow through a highly regulated process. Hematopoietic stem cells within the bone marrow niches differentiate into various progenitor cells, which then mature into specific blood cell types. This process ensures a steady supply of red blood cells for oxygen transport, white blood cells for immune defense, and platelets for clotting.
The hematopoietic stem cell niches in the bone marrow provide the necessary signals and support for the differentiation and production of blood cells. These microenvironments are essential for maintaining the balance and functionality of the hematopoietic system. Any disruption in these niches can lead to impaired blood cell production and various hematological disorders.
Immature vs. Mature Blood Cells
Blood cells mature in the bone marrow, transitioning from immature to mature forms. Immature blood cells, also known as blasts, have not yet developed the full capabilities to function effectively in the body’s systems. As these cells mature, they acquire specific functions necessary for maintaining health, such as oxygen transport by red blood cells and immune responses by white blood cells.
Disruption in the balance of immature and mature blood cells can lead to serious health consequences. For instance, leukemia results in the overproduction of immature white blood cells, which impairs the body’s immune functionality and normal blood cell production.
Knowing the differences between immature and mature blood cells is key for diagnosing and treating blood disorders.
Bone Marrow Diseases
Bone marrow diseases can significantly impact blood cell production, leading to conditions such as anemia, leukopenia, and thrombocytopenia. These diseases disrupt the normal functioning of the bone marrow, resulting in a reduced production of essential blood cells and increasing the risk of infections, bleeding, and other complications.
Early diagnosis and effective treatment of these diseases rely on understanding them.
Aplastic Anemia
Aplastic anemia is a condition where the bone marrow fails to produce enough blood cells. This can be due to various factors, including autoimmune disorders, exposure to toxic chemicals, or certain medications.
Treatments for aplastic anemia include medications to stimulate blood cell production and, in severe cases, bone marrow transplantation to restore healthy blood cell production.
Leukemia and Lymphoma
Leukemia and lymphoma are blood cancers originating in the bone marrow and lymphatic system, respectively. Leukemia results in the production of abnormal leukocytes, which can crowd out normal blood cells in the bone marrow, impairing blood cell production. Common signs of leukemia include fatigue, frequent infections, and easy bruising.
Lymphoma, on the other hand, can lead to the infiltration of lymphatic tissues and abnormal lymphocyte proliferation, impacting hematopoiesis. Symptoms of lymphoma may include swollen lymph nodes and unexplained weight loss.
Both conditions disrupt normal blood cell production and require treatments like chemotherapy, radiation therapy, and bone marrow transplantation to restore healthy blood cell levels.
Multiple Myeloma
Multiple myeloma involves an overproduction of abnormal plasma cells in the bone marrow, interfering with normal blood cell production. This condition leads to damage in bones and a reduction in red blood cell production.
Treatment strategies for multiple myeloma include chemotherapy, targeted therapy, and bone marrow transplants to manage the disease and restore normal bone marrow function.
Bone Marrow Transplants
Bone marrow transplants are a critical treatment option for various hematologic diseases, including certain cancers and genetic blood disorders. These transplants replace damaged or diseased bone marrow with healthy stem cells to restore healthy blood cell production.
This procedure can potentially cure blood-related diseases and significantly enhance patients’ quality of life.
Types of Bone Marrow Transplants
There are two main types of bone marrow transplants: autologous and allogeneic. Autologous transplants use the patient’s own stem cells, which are collected, stored, and reintroduced after intensive treatments such as chemotherapy. This type of transplant reduces the risk of rejection and complications.
Allogeneic transplants involve stem cells from a donor, which can be a relative or an unrelated person. This type of transplant requires careful matching of human leukocyte antigens (HLA) to reduce the risk of graft-versus-host disease, where the donor cells attack the recipient’s body.
Syngeneic transplants, though rare, involve stem cells from identical twins and have the lowest risk of complications.
Pre-Transplant Preparation
Before a bone marrow transplant, patients typically undergo a series of tests to assess their overall health and determine the best transplant type. These evaluations include physical exams, blood tests, and human leukocyte antigen typing to ensure donor compatibility. This phase is crucial for identifying potential risks and planning the procedure.
Preparation may also involve placing a central line and administering conditioning therapy, such as chemotherapy or radiation, to destroy diseased cells and make space for the new stem cells. This phase ensures patients are fit for the procedure and increases the likelihood of a successful transplant.
Post-Transplant Recovery
Recovery after a bone marrow transplant generally takes several months, involving regular follow-ups to monitor for complications and ensure the new stem cells function properly. Patients often risk infections and complications like graft-versus-host disease, where donor cells attack the recipient’s body.
Prolonged medical supervision and staying locally for several weeks may be necessary to monitor recovery and manage potential complications. Recovery can include monitoring for signs of infection, managing side effects, and ensuring that the new bone marrow is producing healthy blood cells.
Support and care during this phase are crucial for a successful transplant outcome.
Bone Marrow Donation
Bone marrow donation can save the lives of patients suffering from blood cancers and other blood disorders. Donating bone marrow provides the stem cells necessary for transplants, offering a chance for recovery and improved quality of life for recipients.
Becoming a donor involves meeting criteria and undergoing health screenings to ensure compatibility with potential recipients.
How to Donate Bone Marrow
To qualify as a bone marrow donor, individuals must meet health criteria and undergo testing to match their human leukocyte antigens (HLA) with patients in need. Potential donors usually need to be between 18 and 44 years old and in good health, as younger donors are often preferred for the success of transplants.
Donating bone marrow typically involves either a bone marrow aspiration through the hip bone or peripheral blood stem cell collection via apheresis. Both methods provide the necessary stem cells for patients requiring transplants.
Prospective donors must pass health screenings and comply with medical guidelines to ensure a successful donation.
Bone Marrow Aspiration and Biopsy
Bone marrow aspiration and biopsy collect bone marrow samples for donation and diagnosis, including a bone marrow biopsy. The collection of bone marrow is typically performed using large needles inserted into the pelvic bones, where the marrow is most abundant. These procedures are essential for diagnosing bone marrow diseases and providing stem cells for transplants.
Aspiration extracts a small amount of liquid marrow, while a biopsy takes a small solid core of marrow tissue. Usually performed under local anesthesia, both procedures critically evaluate bone marrow health and function.
Collected samples assess the composition and condition of the bone marrow, aiding in diagnosis and treatment planning.
Donor Recovery and Care
After donating bone marrow, recovery may include side effects like fatigue, soreness at the needle site, and a need for rest before returning to normal activities. Post-donation recovery usually involves monitoring for any signs of infection and managing pain with over-the-counter medication. Most donors can resume regular activities within a few days, though complete recovery may take about 20 days.
Donors may experience soreness at the collection site and should avoid heavy activities for a few days to aid recovery. Care and support during recovery are essential for a smooth and successful donation experience.
Donating bone marrow is a generous act that saves lives; the recovery process is a small price for its immense impact on patients in need.
Bone Marrow and the Immune System
Bone marrow is crucial for developing and maturing lymphocyte populations, such as B cells and T cells, vital for effective immune responses. These immune cells play critical roles in maintaining health and protecting the body against pathogens and diseases.
Producing lymphocytes in the bone marrow ensures a robust and functional immune system capable of responding to various infections and illnesses.
White Blood Cells
White blood cells, or leukocytes, are essential components of the immune system, produced in the bone marrow through hematopoiesis. Hematopoietic stem cells in the bone marrow differentiate into various white blood cells, including granulocytes, lymphocytes, and monocytes. Granulocytes include neutrophils, eosinophils, and basophils, each playing a unique role in the immune response.
Adults produce around 100 billion blood cells daily, highlighting the importance of a healthy and functioning bone marrow. Immature blood cells gradually differentiate into specific types, ensuring a steady supply of immune cells and platelets necessary for maintaining defenses and overall health.
Lymphocytes
Lymphocytes, produced in the bone marrow, play crucial roles in both innate and adaptive immunity. These include B cells, which create antibodies, T cells that help regulate immune responses and attack infected or cancerous cells, and natural killer (NK) cells that target and eliminate virus-infected cells. Each type of lymphocyte has a specific function that is essential for a comprehensive immune response.
Immature blood cells, or blasts, have not yet developed the full capabilities to function in the immune response compared to only mature blood cells. Maturation within the bone marrow ensures lymphocytes and other immune cells are fully equipped to protect against infections and diseases.
Maintaining healthy bone marrow is vital for a robust and effective immune system.
Bone Marrow Health and Maintenance
Maintaining healthy bone marrow requires a balanced diet, regular exercise, and avoiding harmful substances. Healthy bone marrow is essential for producing blood cells needed for functions like oxygen transport, immune defense, and blood clotting.
Following these guidelines supports your bone marrow’s health and ensures its optimal function.
Nutritional Support
A balanced diet rich in vitamins and minerals is crucial for maintaining bone marrow health. Essential nutrients like iron, folic acid (B9), and vitamin B12 are crucial for producing healthy blood cells in the bone marrow. Foods like wheatgrass, turkey, and lentils are particularly beneficial for enhancing bone marrow health.
Wheatgrass is highly regarded for its rich nutrient profile, turkey provides essential proteins and vitamins, and lentils are an excellent source of folic acid vital for generating red blood cells. Incorporating these foods into your diet can help maintain a healthy bone marrow and ensure the continuous production of new blood cells.
Avoiding Toxins
Exposure to environmental pollutants can adversely affect bone marrow health, making it essential to minimize such risks. Harmful substances like heavy metals (e.g., lead) and certain chemicals can negatively impact bone marrow function. Avoiding exposure to these toxins is crucial for protecting your bone marrow and ensuring its proper function.
Minimizing exposure to harmful environmental substances can help protect bone marrow function. Simple steps such as avoiding smoking, reducing exposure to industrial pollutants, and using protective equipment when handling chemicals can significantly reduce the risk of bone marrow damage.
Maintaining a toxin-free environment supports overall health and well-being.
Regular Check-ups
Routine medical examinations are important for the early detection of potential bone marrow-related disorders. Regular check-ups can help identify issues such as anemia, leukopenia, or thrombocytopenia early, allowing for timely intervention and treatment. Early detection of bone marrow disorders can significantly improve treatment outcomes and prevent complications.
Regular medical evaluations can help identify potential bone marrow disorders early, improving treatment outcomes. These check-ups are key for maintaining overall health and ensuring that your bone marrow continues to function effectively. By staying proactive with your health, you can support your bone marrow and overall well-being.





