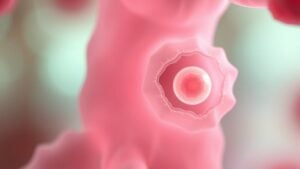
Granulosa cells are essential players in female fertility, quietly working behind the scenes to support oocyte development and hormone production in ovarian follicles. These cells do far more than merely occupy space; they actively engage in estrogen synthesis and signal to the oocyte through intricate communication networks. However, if these cells malfunction, it can lead to serious conditions such as PCOS or premature ovarian failure. Grasping their role is vital for maintaining reproductive health and managing treatment options effectively. What lies ahead in the world of granulosa cell research could reveal unexpected discoveries for many.
Overview of Granulosa Cells
Granulosa cells play a pivotal role in female fertility, serving as the supportive structure for oocytes within ovarian follicles. These cells are essential for follicular development and steroid hormone production, particularly estradiol, as they convert androgens from theca cells through aromatase, a process tightly regulated via FSH signaling.
As follicles progress through development stages—from primordial to antral—granulosa cells multiply and differentiate, creating a nurturing environment for oocyte maturation. Significantly, they communicate directly with oocytes through gap junctions, enhancing growth and maturation.
At times follicles do not dominate, granulosa cells undergo apoptosis, leading to follicular atresia. This ever-changing balance between growth and degeneration highlights their significance in maintaining female reproductive health.
Key Functions of Granulosa Cells
The functions of granulosa cells extend far beyond merely supporting oocyte development; they are active players in the ovarian environment that directly influence female fertility. Their crucial roles include:
- FSH Receptor Activation: Granulosa cells respond to Follicle Stimulating Hormone (FSH), leading to increased cell proliferation and differentiation, essential for follicular development.
- Estrogen Production: Through converting androgens via steroidogenic enzymes, granulosa cells produce estradiol, markedly higher than in theca cells, enhancing oocyte maturation.
- Regulating Apoptosis: Apoptosis of granulosa cells is essential for managing follicular atresia, tightly regulated by various growth factors.
Through these functions, granulosa cells not only support the growth of healthy eggs but also help maintain a balanced ovarian environment critical for general fertility.
Estrogen Production and Regulation
While the role of estrogen in the female body is often recognized for its association with fertility and reproductive health, the process of its production is closely linked to the cooperation between distinct cell types within the ovary. Granulosa cells and theca cells function together through a two-cell system. Theca cells generate androgens, which granulosa cells transform into estradiol via aromatase (CYP19A1) under FSH stimulation. This cAMP/PKA signaling elevates estradiol output markedly during the follicular phase maturation, participating in the LH surge.
| Cell Type | Key Function | Regulation |
|---|---|---|
| Granulosa | Aromatize androgens to estradiol | FSH-dependent |
| Theca | Produce androgens | LH-dependent |
| Follicular Phase | Peak estradiol production | Feedback mechanisms |
Granulosa Cells in Ovarian Folliculogenesis
In the intricate progression of ovarian folliculogenesis, granulosa cells assume a fundamental role, far beyond just synthesizing estrogen. These cells markedly support follicular growth through various mechanisms, including:
- Proliferation: Granulosa cells increase from approximately 15 in primordial follicles to about 50,000 in preovulatory follicles.
- Estradiol Synthesis: Through converting androgens from theca cells, they produce peak levels of estradiol, essential for ovulation.
- Regulating Survival: Apoptosis in granulosa cells leads to follicular atresia, with many follicles degenerating whenever survival signals like FSH and IGF1 are disrupted.
In dominant follicles, granulosa cells boost their responsiveness to gonadotropins by upregulating FSHR and LHCGR, ensuring successful maturation and ovulation. Therefore, their functions are vital for ongoing fertility.
Hormonal Interactions and Signaling Pathways
Hormonal interactions within granulosa cells are crucial for reproductive success, emphasizing the cooperation between insulin-like growth factor (IGF) and follicle-stimulating hormone (FSH).
This collaboration enhances signaling pathways that regulate critical processes, including GC differentiation and ovulation readiness.
Additionally, the influence of fibroblast growth factor (FGF) and interleukin-7 (IL7) further highlights the intricate network of hormonal communication essential for follicular development.
IGF and FSH Synergy
Granulosa cells play a central role in female fertility, particularly through the intricate interplay of insulin-like growth factor 1 (IGF1) and follicle-stimulating hormone (FSH). This collaboration improves various aspects of follicular maturation:
- IGF1 amplifies FSH-induced production of steroidogenic enzymes like StAR and aromatase, vital for estradiol synthesis.
- FSH stimulates the expression of IGF1 receptors in granulosa cells, facilitating IGF1-mediated follicular growth.
- Both hormones collaboratively activate the PI3K/AKT pathway, promoting the survival and proliferation of granulosa cells.
Moreover, FSH regulates PAPP-A, which decreases IGFBP levels, thereby increasing IGF availability.
Through these mechanisms, IGF1 and FSH create a supportive environment for ideal follicular development and comprehensive reproductive health, encouraging improved fertility results.
FGF Influence on GC
While studying the fascinating world of follicular development, the influence of fibroblast growth factors (FGFs) on granulosa cells becomes a key aspect to investigate. FGFs play an essential role in ovarian function through regulating steroid hormone production.
For instance, FGF2 can suppress estradiol production while enhancing progesterone synthesis in specific cell cultures of rat granulosa cells. Additionally, FGF7 exhibits inhibitory effects on hormone production in various species, illustrating its species-specific roles.
Importantly, FGF9 presents a contrasting effect on estradiol synthesis, emphasizing the complexity of FGF signaling pathways in granulosa cells. These interactions help shape follicular fluid dynamics and general follicular health, showcasing the delicate interplay between growth factors and ovarian hormone regulation.
IL7 Signaling Mechanisms
Fibroblast growth factors aren’t the only players in the complex game of follicular development. Interleukin-7 (IL7) plays a central role in enhancing granulosa cell function, influencing several key processes critical for ovarian health.
Its signaling mechanisms operate via:
- Activation of the JAK/STAT pathway, leading to increased cell survival and proliferation.
- Modulation of steroidogenic enzyme expression, particularly enhancing CYP19A1, elevating estradiol production.
- Regulation of apoptosis via inhibiting caspase-3 activity through PI3K/AKT activation, reducing cell death in challenging conditions.
Impact of Dysregulated Granulosa Cells on Fertility
At the time of considering the intricate dance of fertility, it becomes clear that dysregulated granulosa cells play a major role in this process. Impaired steroidogenesis in these cells often results in reduced estradiol production, disrupting follicular development and ovulation.
Granulosa cells undergo abnormal apoptosis, especially in atretic follicles, contributing to premature ovarian failure and decreased ovarian reserve. Additionally, cells obtained from infertile women show lower expression of FSH receptors, hampering their maturation during IVF treatments.
Moreover, oxidative stress increases in granulosa cells, particularly in conditions like endometriosis. This can lead to DNA damage and compromised oocyte quality.
Finally, insulin-resistant granulosa cells in polycystic ovary syndrome overproduce androgens, inhibiting follicle development and substantially raising anovulation risks.
Associated Conditions With Granulosa Cell Dysfunction
Granulosa cell dysfunction is intricately linked to various reproductive health conditions, making it a crucial area to investigate for anyone facing fertility challenges. Key associated conditions include:
- Polycystic Ovary Syndrome (PCOS): About 50-70% of women with PCOS experience altered FSH receptor expression and impaired steroidogenesis due to granulosa cell issues.
- Premature Ovarian Failure (POF): This condition primarily results from granulosa cell apoptosis, affecting 60-80% of cases where follicular development is abnormal.
- Granulosa Cell Tumors (GCTs): Representing 2-5% of ovarian cancers, GCTs can disrupt fertility through excessive hormone production.
Additionally, diminished ovarian reserve (DOR) often indicates reduced granulosa cell proliferation, while oxidative stress, particularly in endometriosis, further complicates fertility results.
Grasping these conditions highlights the significance of granulosa cell health in reproductive success.
Therapeutic Approaches for Granulosa Cell Disorders
Therapeutic approaches for granulosa cell disorders encompass various strategies customized to improve fertility and address tumor challenges.
Surgical interventions, particularly for granulosa cell tumors, often lead to encouraging fertility results, while hormonal therapies can support follicular development in affected individuals. Additionally, comprehending recurrence rates is crucial for ongoing management and patient assurance. New treatments are being developed that target granulosa cell function, aiming to enhance reproductive potential and mitigate complications related to granulosa cell disorders.
Surgical Interventions for Tumors
At the time of considering surgical interventions for granulosa cell tumors, several approaches can be employed to effectively manage the condition while aiming to preserve fertility. Primary treatments typically include:
- Ovariectomy: Removing the affected ovary, allowing for potential fertility preservation provided the other ovary is healthy.
- Laparoscopic Techniques: Employing minimally invasive surgery to reduce recovery times and complications.
- Monitoring: Regular serum anti-Müllerian hormone (AMH) level checks post-surgery to detect any signs of recurrence.
In cases of bilateral granulosa cell tumors, bilateral oophorectomy might be necessary, followed by hormone replacement therapy to alleviate menopausal symptoms.
These surgical interventions highlight the commitment to balancing effective treatment with the imperative of maintaining fertility.
Hormonal Therapy Considerations
Fertility preservation through hormonal therapy represents a promising avenue for managing granulosa cell disorders. Through the use of FSH and LH analogs, healthcare providers can stimulate granulosa cell proliferation and steroidogenesis, resulting in a 60-70% success rate for ovulation induction, particularly in PCOS patients.
Aromatase inhibitors, like letrozole, effectively lower excessive estrogen production, showing a 27.5% improvement in ovulation rates compared to clomiphene citrate. Additionally, GnRH antagonists prevent premature luteinization, enhancing IVF success rates by 15-20%.
For those experiencing luteal phase defects, progesterone supplementation post-ovulation is vital, as it supports granulosa cell function, improving endometrial receptivity and reducing initial pregnancy loss. These therapeutic strategies provide hopeful options for individuals facing fertility challenges linked to granulosa cell disorders.
Monitoring Recurrence Rates
Monitoring the recurrence of granulosa cell disorders is vital for maintaining continued health and wellness following initial treatment. Grasping the recurrence rates can inform suitable postoperative surveillance approaches. The following factors are pivotal in this process:
- Serum inhibin B levels: Levels surpassing 100 pg/mL are notable for identifying recurrence.
- FDG-PET/CT imaging: This diagnostic technique demonstrates 92% sensitivity in detecting recurrences, surpassing traditional imaging methods.
- Long-term follow-up: Research reveals a 10-30% recurrence rate, frequently emerging 4-6 years after diagnosis, requiring routine evaluations every six months.
Employing adjuvant chemotherapy may also reduce the recurrence risk by 40% in certain stages, highlighting the importance of an all-encompassing monitoring strategy customized to individual needs.
Future Research Directions in Granulosa Cell Biology
Exploring the future of granulosa cell biology opens up an exciting domain of possibilities for boosting fertility treatment and comprehending ovarian health. Research is pivoting towards granulosa cell-derived extracellular vesicles, which could serve as biomarkers for ovarian reserve. Single-cell RNA sequencing aims to reveal distinct subpopulations of steroidogenic cells. Additionally, CRISPR technology is being employed to pinpoint specific gene expression pathways that contribute to ovarian dysfunction. Investigating mitochondrial transfer from granulosa cells to oocytes could further elevate IVF results. Moreover, evaluating senescence mechanisms will pave the way for anti-aging therapies.
| Research Focus | Key Techniques | Potential Impact |
|---|---|---|
| Extracellular vesicles as biomarkers | miRNA analysis | Predict fertility results |
| Single-cell RNA sequencing | Characterization of GC | Identify functional clusters |
| CRISPR-Cas9 gene editing | Pathway targeting | Model ovarian dysfunction |
| Mitochondrial transfer | ATP quantification | Improve IVF efficiency |
Importance of Granulosa Cells in Reproductive Health
Granulosa cells play a pivotal role in maintaining reproductive health, acting as the nurturing environment for developing oocytes. These indispensable cells support ovarian follicles by facilitating key processes:
- Hormone Production: Granulosa cells synthesize estradiol, essential for follicle maturation.
- Follicle Growth: Through binding with FSH, they drive the growth of follicles required for ovulation.
- Regulating Oocyte Health: They protect developing oocytes via apoptosis regulation, ensuring proper selection of viable follicles.
Their significance becomes even clearer in conditions like PCOS, where GC dysfunction can lead to anovulation, affecting fertility.
Comprehending the role of granulosa cells helps illuminate their impact on overall reproductive wellness, creating pathways for targeted treatments and enhanced health results.