The connection between irritable bowel syndrome and sleep runs deeper than midnight bathroom trips. Research shows gut inflammation disrupts melatonin production, while bloating and cramping make it hard to settle into restful sleep. Many with IBS experience frequent awakenings or struggle to fall asleep, creating a frustrating cycle where poor sleep worsens digestive symptoms the next day.
Grasping this link opens doors to better management but initially, let’s unpack why the gut and brain keep each other awake.
The Gut-Brain Axis and Sleep
Provided the gut and brain aren’t communicating well, sleep often pays the price. The gut-brain axis links digestive health to sleep quality, and when this connection falters, IBS symptoms like cramping or bloating can disrupt rest. Inflammation in the gut might interfere with melatonin production, the hormone regulating sleep, leading to restless nights.
Inadequate sleep quality then worsens gut health, creating a cycle of discomfort. Nearly half of IBS patients report trouble falling or staying asleep, as pain and discomfort make relaxation difficult. Even without official diagnostic ties, sleep disturbances frequently accompany IBS, highlighting how deeply gut health impacts overall well-being.
Comprehending this connection helps explain why managing IBS symptoms often improves sleep—and vice versa. Prioritizing both gut and sleep health can break the cycle.
Pain-Related Sleep Disturbances in IBS Patients
Pain keeps many IBS patients awake at night, turning what should be restful sleep into a struggle. Abdominal pain, a hallmark of IBS, often worsens at night, making it harder to relax and fall asleep.
Many with IBS live with frequent sleep disturbances, waking up due to discomfort from diarrhea and abdominal cramps. These pain-related sleep disturbances don’t always shorten total sleep time but make rest less invigorating. Inadequate sleep can then worsen IBS symptoms, creating a frustrating cycle.
While constipation and diarrhea play a role, pain remains the biggest disruptor. For those managing IBS, nighttime discomfort isn’t just physical—it steals the chance to wake up feeling rejuvenated. Comprehending this link helps IBS patients seek better strategies to improve both digestion and sleep quality.
The Role of Inflammation in IBS and Sleep Quality
Inflammation in the gut can interfere with sleep by disrupting the body’s natural rhythms, while poor sleep can further increase inflammation, worsening IBS symptoms.
This cycle creates a challenging loop where digestive discomfort and restless nights feed into each other. Managing inflammation through lifestyle changes or treatments could help break this pattern and improve both gut health and sleep quality.
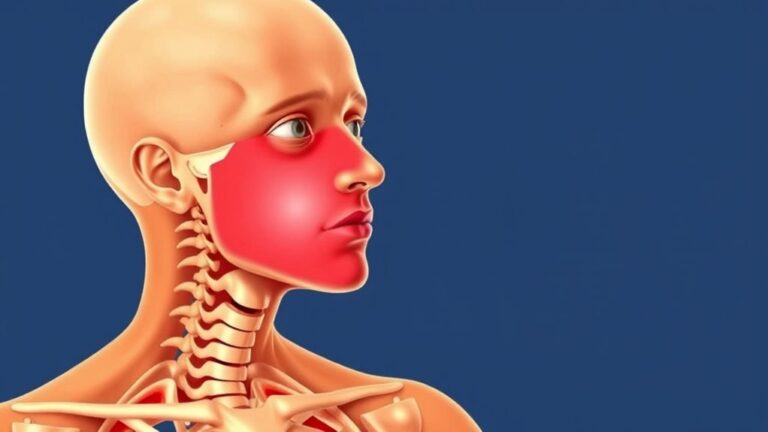
Gut Inflammation Disrupts Sleep
Since gut irritation and poor rest often feed into each other, knowledge of how inflammation disturbs sleep is key for those with irritable bowel syndrome. Elevated inflammatory markers like TNFα in IBS patients can disrupt the body’s circadian rhythm, leading to sleep disturbances.
An unbalanced gut microbiome might further worsen inflammation, creating a cycle where digestive health impacts sleep quality. Nighttime IBS symptoms—cramping, urgency, or bloating—can also interrupt sleep, making chronic sleep deprivation a common struggle.
Addressing inflammation through better sleep hygiene, such as consistent bedtimes and reducing late-night meals, could help. Managing digestive health with dietary adjustments and stress reduction might also ease inflammation, improving rest.
Breaking this cycle requires understanding how deeply gut inflammation and sleep intertwine for those with IBS.
Sleep Loss Worsens IBS Inflammation
A restless night can do more than leave someone groggy—it could also fuel digestive distress for those with IBS. Sleep deprivation raises inflammatory markers like TNFα, which disrupts sleep-wake cycles and worsens gut inflammation.
Poor sleep quality creates a vicious cycle, where higher inflammation levels intensify IBS symptoms, making rest even harder to achieve. Studies show that balancing gut health and sleep is crucial, as reducing inflammation improves both digestion and rest.
Simple lifestyle changes—like consistent sleep schedules, stress management, and anti-inflammatory foods—can help break this loop. Treatment approaches focusing on both sleep and gut health, such as cognitive behavioral therapy for insomnia or probiotics, might offer relief.
Addressing inflammation through balanced habits could ease discomfort and restore restful nights.
Co-Occurring Sleep Disorders Among IBS Sufferers
Research highlights a strong link between IBS and sleep disorders, with insomnia and hypersomnia symptoms being markedly more common in this group.
People with IBS are over twice as likely to experience sleep problems compared to those without digestive issues, affecting their daily energy and focus.
These disruptions often create a cycle where poor sleep worsens IBS symptoms, and digestive discomfort further harms rest.
IBS and Insomnia Connection
Digestive discomfort isn’t the only struggle for those with irritable bowel syndrome—sleep often takes a hit, too. Research shows people with IBS are 3.1 times more likely to experience insomnia, with poor sleep quality worsening bowel symptoms.
The link between sleep and IBS symptoms is strong: nighttime pain, urgency, or bloating can disturb your sleep, while lack of sleep heightens gut sensitivity. Anxiety and depression, common in IBS, further disrupt the circadian rhythm, creating a cycle of sleep issues.
Cortisol spikes from stress also lower the quality of sleep, leaving many exhausted. Addressing sleep hygiene—like consistent bedtimes and limiting caffeine—can help break this loop. For those with IBS, prioritizing rest isn’t just about energy; it’s a key part of managing gut health.
Sleep Disorder Prevalence Rates
Sleep disorders don’t just occasionally trouble those with IBS—they’re far more common than many recognize. Research shows a robust co-occurrence between gastrointestinal disorders like IBS and disrupted sleep patterns, with nearly 38% of IBS patients also experiencing sleep disorders. This connection highlights how digestive health directly impacts sleep quality.
Insomnia is 3.1 times more likely in IBS sufferers, often due to nighttime discomfort or stress. Hypersomnia (excessive sleepiness) is 4.6 times more frequent, possibly linked to fatigue from poor rest. Children with IBS face seven times higher rates of sleep disturbances, underscoring early-life impacts.
The overlap between IBS and sleep disorders suggests shared mechanisms, like gut-brain axis dysfunction. Addressing one could improve the other, emphasizing the need for comprehensive care.
Impact on Daily Functioning
Many people with IBS don’t just struggle with digestive symptoms—their sleep suffers too, and that can make everyday life feel like an uphill battle. Research has found a strong link between IBS and poor sleep quality, with patients reporting fewer restful hours due to conditions like insomnia or hypersomnia.
This lack of sleep can worsen fatigue, focus, and mood, making it harder to manage daily tasks. People with IBS often report feeling exhausted, even after what should be sufficient sleep. Co-occurring conditions like anxiety or depression further disrupt sleep, creating a cycle that’s tough to break.
Improving sleep habits can help, but it’s crucial to address both digestive and sleep issues together for better overall functioning.
How IBS Subtypes Affect Sleep Patterns
Certain IBS subtypes create unique challenges at the time it comes to getting restful sleep. IBS-C (constipation-predominant) often delays sleep onset due to discomfort, while IBS-D (diarrhea-predominant) disrupts sleep with frequent nighttime awakenings. IBS-M (mixed) combines both issues, further fragmenting the sleep-wake cycle. Digestive symptoms like bloating, cramping, or urgency directly interfere with sleep quality, leaving individuals fatigued.
- IBS-C: Prolonged sleep onset from abdominal pressure.
- IBS-D: Repeated bathroom trips break sleep continuity.
- IBS-M: Unpredictable symptoms destabilize the sleep-wake cycle.
Managing these symptoms—through diet, hydration, or medications—can minimize sleep disturbances. Recognizing how each IBS subtype affects rest helps tailor solutions for better sleep hygiene and overall well-being.
Sleep Apnea and Its Connection to Digestive Health
Breathing troubles during sleep can do more than just leave someone weary the next day—they could also exacerbate digestive issues like IBS. Studies show people with sleep apnea often experience more severe IBS symptoms, as interrupted sleep affects gut function.
Researchers found these changes in sleep patterns may trigger inflammation or stress responses, further disrupting digestion. About 20% of people struggle with sleep apnea, marked by snoring, gasping for air, or dry mouth. Should IBS symptoms persist, discussing sleep apnea with a healthcare provider could be crucial.
Proper treatment, like using a CPAP machine, might enhance both sleep and overall health. Addressing sleep apnea may ease digestive discomfort, highlighting how closely IBS and sleep are linked. Timely intervention can make a difference.
Mood Disorders and Sleep Challenges in IBS
Sleep issues don’t just stem from physical discomfort—they often tie closely to mood. For those with IBS, mood disorders like anxiety and depression can worsen sleep at night, creating a cycle where insufficient sleep further disrupts mental health conditions. The nervous system becomes overactive, making consistent sleep harder to achieve.
Uncontrolled psychiatric symptoms, such as racing thoughts or heightened stress, make staying asleep a challenge, lowering overall quality of life.
- Anxiety and depression often accompany IBS, heightening nighttime wakefulness.
- Digestive discomfort like abdominal pain can trigger awakenings, fragmenting rest.
- Stress responses keep the body alert, delaying deep sleep phases.
Addressing both digestive and mental health is key to breaking this cycle. Consulting a healthcare provider for tailored treatment can improve sleep and daily well-being.
Dietary and Lifestyle Strategies for Better Sleep
Mindful eating habits can reduce digestive discomfort that disrupts sleep, such as chewing slowly and avoiding late meals.
Stress reduction techniques, like deep breathing or gentle stretching, can calm both the gut and the mind before bedtime.
Small adjustments in daily routines often help ease IBS symptoms and improve rest.
Mindful Eating Habits
Managing IBS-related sleep issues starts with paying attention to what and how you eat. Mindful eating habits can ease digestive discomfort and improve rest by supporting the gut microbiota. A Low FODMAP diet might/could reduce bloating and gas, while avoiding caffeine late in the day prevents sleep disruptions. Small dietary changes, like eating slower and chewing thoroughly, help the digestive system process food more efficiently.
Track trigger foods: Keeping a food diary identifies patterns between meals and sleep disturbances.
Limit late-night meals: Eating earlier allows the gut bacteria to settle before bedtime.
Consider melatonin supplements: Taking melatonin before bed can/might regulate sleep cycles disrupted by IBS.
Lifestyle changes, such as mindful eating habits, create a calmer digestive environment, promoting better sleep.
Stress Reduction Techniques
Many people with IBS find that stress worsens their symptoms, making it harder to unwind at night. Studies show that poor sleep and gut health are closely linked, increasing the chance of developing IBS or greatly affecting symptoms for those already affected.
People with IBS often report having sleep problems, which can further disrupt digestion. To improve sleep, limiting daytime naps to 30 minutes helps maintain nighttime rest. Avoiding caffeine and nicotine before bed prevents stimulation, while daily exercise—but not too close to bedtime—supports deeper sleep.
Exposure to natural light regulates the sleep-wake cycle, and a dark, quiet bedroom with comfortable bedding encourages relaxation. These small changes can profoundly affect sleep quality, easing discomfort for those with inflammatory bowel disease or IBS.
Medical Treatments to Improve Sleep for IBS Patients
Several treatment options exist to help IBS patients struggling with sleep disruptions. A healthcare professional may suggest a personalized treatment plan, which could include medications like antidepressants, antihistamines, or benzodiazepines to address both digestive discomfort and sleep issues.
Melatonin supplements may also help regulate the sleep-wake cycle while easing abdominal pain. Cognitive behavioral therapy (CBT) can be effective for insomnia linked to IBS by targeting stress and negative thought patterns. In some cases, sleep studies might be required to identify underlying disorders like sleep apnea.
- Medications: Antidepressants or antihistamines may improve sleep quality and reduce IBS symptoms.
- Supplements: Melatonin can aid in regulating sleep cycles.
- Therapy: CBT helps manage stress and insomnia.
Always consult a doctor before starting any new treatment to confirm safety and effectiveness.
The Bidirectional Relationship Between Gut Health and Rest
The connection between gut health and sleep goes both ways. The link between IBS and sleep quality is a bidirectional relationship: poor gut health disrupts rest, and poor rest worsens digestive issues.
Those with IBS tend to experience significant sleep problems, like frequent nighttime awakenings or difficulty falling asleep, which lower overall quality of life. Conversely, lack of sleep can cause problems like increased gut inflammation, making IBS symptoms worse.
To break this cycle, tips to improve both sleep and health include sticking to a regular bedtime, avoiding heavy meals before bed, and managing stress. Addressing one issue often helps the other, creating a positive ripple effect. Recognizing this connection is key to finding balance in both gut and sleep health.
Conclusion
Residing with IBS can feel like fighting a nightly battle where gut and sleep pit against each other. Yet comprehension of their connection lights a path toward better nights. As digestion calms, rest often follows—breaking the vicious cycle piece by piece. Small diet shifts, stress tools, and gut-supporting habits rebuild the foundation for deeper sleep. Where discomfort once ruled, steadier nights become possible again, one gentle change at a time.