Subacromial decompression is for shoulder pain caused by impingement. It is the best option for you after you failed shoulder treatment.
Of course, your surgeon will use arthroscopic technique, small camera and instruments that are less invasive on your body. Thus, one study found that there was an 8.1% rate of complications during arthroscopic treatments, while open surgeries had a 6.6% rate. This difference was not significant.
Here we’ll explain what happens, why you need it and what to expect during recovery.
What is subacromial decompression?
Subacromial decompression surgery is a targeted treatment for impingement syndrome. Impingement syndrome occurs when the tendons and bursa in the subacromial space (where the humerus, scapula, and clavicle meet) become pinched and inflamed. The surgery increases this space, reducing the compression and the pain.
The procedure involves trimming away some of the acromion bone and removing any bony spurs that are contributing to the impingement. This allows the tendons to move more freely without getting pinched, reducing pain and improving shoulder function.
Subacromial decompression surgery is an option when physical therapy and anti-inflammatory medications don’t work.
It’s a way to restore mobility and reduce pain for those with chronic impingement so you can get back to your daily activities without discomfort.
The Surgical Procedure
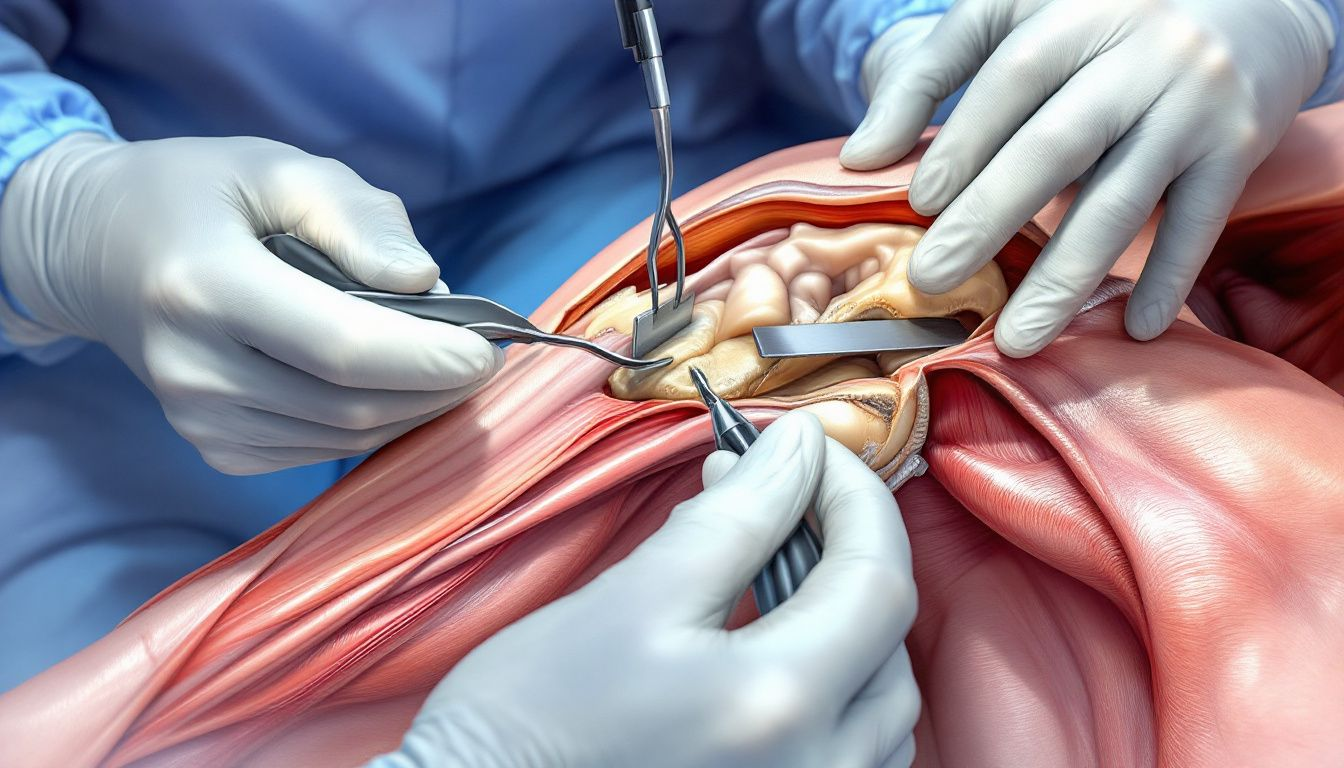
Subacromial decompression surgery can be done arthroscopically (keyhole) or through an open incision. Arthroscopic is preferred as it’s minimally invasive and involves small incisions and specialized instruments.
The main aim of the procedure is to relieve pressure on the rotator cuff tendons by removing inflamed tissue and bone spurs.
The following sections will go into the arthroscopic technique, keyhole operation, general anesthesia, and nerve blocks for pain management.
Arthroscopic Surgery
Arthroscopic subacromial decompression surgery involves small incisions and specialized instruments. Key instruments are an arthroscope, a tiny camera that guides the surgeon, and a shaver for removing inflamed bursa and trimming bone spurs.
The surgeon checks the rotator cuff tendons to see if there are any other issues that need to be addressed. This thorough check of the rotator cuff helps prevent future complications and ensures the success of the surgery.
Keyhole Operation
Keyhole surgery involves small incisions for the instruments. A video camera guides the surgeon to remove bone spurs and inflamed bursa. This minimizes tissue damage and faster recovery.
Small incisions reduces infection risk and complications, it’s a safe and effective way to do shoulder decompression. Patients have less post-op pain and faster healing time compared to open surgery.
General Anesthetic and Nerve Block
The surgery is done under general anesthetic, the patient is unconscious and pain-free. A nerve block is often given to manage postoperative pain.
The nerve block takes about 10 minutes to place and numbs the shoulder area and provides good pain relief as the patient wakes up.
Post-Op Expectations
The surgery relieves pressure on the rotator cuff tendons by removing inflamed tissue and bone spurs. Patients can expect significant pain reduction and improved shoulder mobility if they follow the recovery protocols.
Recovery includes immediate post-op care and long-term rehabilitation. Patients should follow their surgeon’s instructions, do physical therapy and modify their activities to prevent further injuries.
Immediate Recovery Phase
After surgery, patients are advised to use a shoulder sling for the first 24 hours. The sling is worn for 1-3 days, then gentle movement is done to prevent stiffness. Painkillers manage the pain and ice packs reduces swelling and pain.
Early movement prevents complications like post-op frozen shoulder or adhesive capsulitis. Inadequate shoulder movement can cause stiffness and prolonged recovery. Anti-inflammatory medications can be taken as needed to manage swelling.
Long-term Rehabilitation
Long-term rehabilitation is key to full recovery. Physical therapy focuses on exercises to strengthen the shoulder, alleviate pain and improve mobility.
Physical therapy starts with immobilization then passive and active exercises. Recovery from shoulder decompression surgery usually takes 4 months.
As you can see, full recovery time varies from individual to individual. Significant improvement is seen within 3 months and continued progress within 12 months.
Returning to sports and other activities is possible once full, pain-free movement is achieved.
Factors like type of sport, strength, and range of motion will determine the timeline to return to activities.
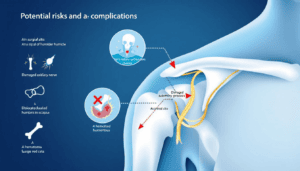
Risks and Complications
Like any surgery, subacromial decompression has risks and complications.
Here are the risks to watch out for:
- Infection: Monitor for symptoms post-op and seek medical attention if symptoms arise.
- Peripheral nerve injuries: Rare but can happen and may be temporary or permanent.
- Serious complications: Deep infection and pulmonary embolism are less than 1%.
Surgical vs. Non-Surgical Options
According to recent studies, shoulder impingement exercises are effective in restoring shoulder mobility and reducing chronic pain in a significant number of patients. For instance, a study reported functional improvement in 90% of cases following physiotherapy interventions for shoulder impingement syndrome.
For shoulder impingement syndrome patients have surgical and non-surgical options. Conservative measures like anti-inflammatory medications and physical therapy are usually the first line of treatment for shoulder pain and gives significant relief to many patients.
When conservative treatment fails to relieve symptoms, subacromial decompression surgery becomes an option. The surgery is beneficial for active adults who still have pain despite nonsurgical interventions.
Here’s the options:
- Conservative measures: Anti-inflammatory medications and physical therapy.
- Surgery: When nonsurgical options fail.
- Benefit: Active adults.
Must consult with a healthcare professional to determine the best course of action.
Follow-Up Care
Regular check-ups allows clinicians to monitor tendon healing and shoulder function to early detect and address complications.
Having someone to assist at home the first night post-op is important for comfort and to follow instructions.
Wrap Up
At the end of the day, Subacromial decompression surgery is a good tool to address shoulder impingement syndrome, gives relief from pain and restore shoulder function.